Gout Medication Selector
Gout Medication Selection Guide
Answer the following questions to find the best urate-lowering therapy for your condition:
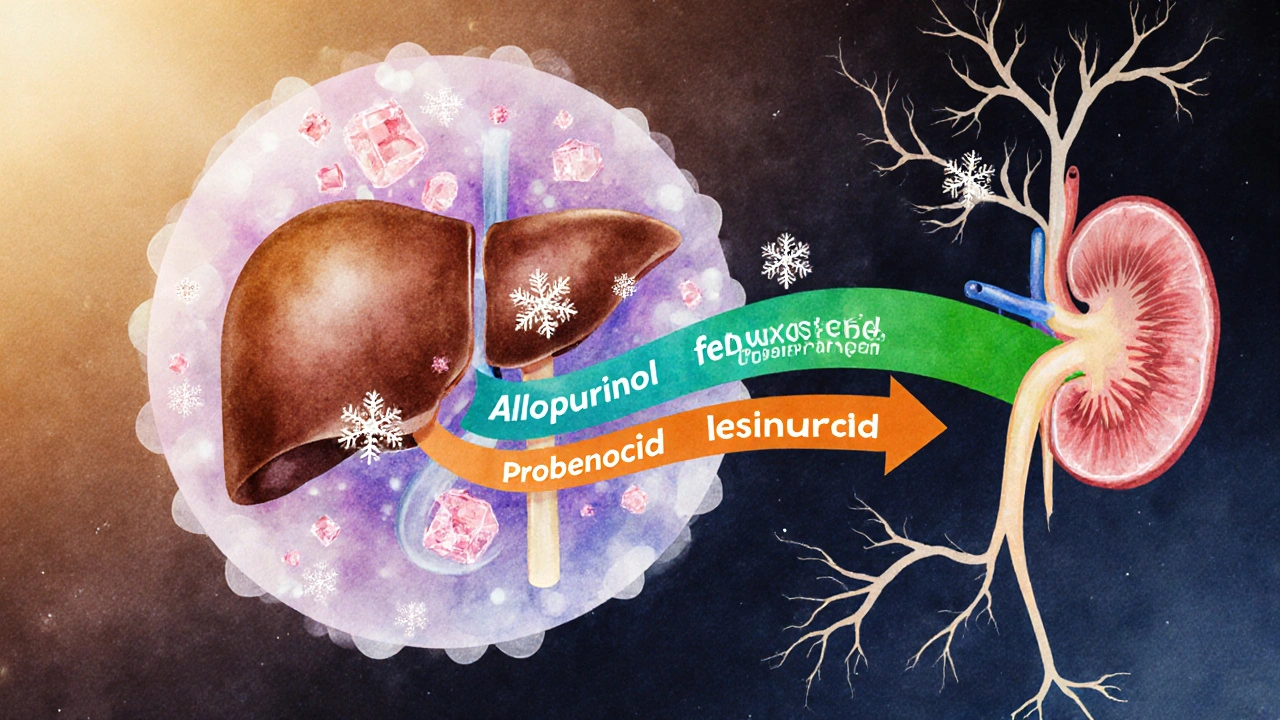
TL;DR
- Allopurinol (Zyloprim) is the first‑line urate‑lowering drug but can cause rash, dose‑dependent kidney issues, and interactions.
- Febuxostat works similarly but is safer for patients with mild‑moderate renal impairment; watch for cardiovascular warnings.
- Probenecid is a uricosuric that helps kidneys dump uric acid; not suitable if you have kidney stones or severe CKD.
- Lesinurad is added to a xanthine oxidase inhibitor (usually allopurinol or febuxostat) to boost uric‑acid clearance; watch for sudden kidney injury.
- Pegloticase and topiroxostat are third‑line options for refractory gout; peg‑ is IV, topiroxostat is oral and used in Japan/Europe.
What is Zyloprim (Allopurinol)?
When you hear the name Allopurinol a xanthine oxidase inhibitor that reduces uric‑acid production, think of the drug that’s been the backbone of gout therapy since the 1960s. Sold under the brand Zyloprim, it blocks the enzyme that converts purines into uric acid, keeping blood levels in check and preventing painful flares.
Typical dosing starts at 100mg daily, climbing to 300mg or even 600mg in resistant cases. Most people tolerate it well, but the drug isn’t without quirks: a hypersensitivity rash (often called “allopurinol hypersensitivity syndrome”) can be life‑threatening, especially in patients with renal impairment or on high doses. That’s why many look for Allopurinol alternatives when side‑effects or drug interactions become a problem.
Why Seek Alternatives?
Gout isn’t just a toe‑pain story; it can lead to kidney stones, joint damage, and cardiovascular strain. While allopurinol works for ~80% of patients, several scenarios push you toward other options:
- Kidney disease: Allopurinol dose‑adjusts poorly; higher doses raise toxicity risk.
- Drug interactions: Concurrent azathioprine or warfarin may need dose tweaks.
- Allergy or rash: Even a mild skin reaction may signal a severe hypersensitivity later.
- Inadequate urate control: Some patients never hit the target <120µmol/L
When one of these flags pops up, clinicians weigh the pros and cons of other urate‑lowering agents. Below is a quick snapshot of the most common alternatives.
Febuxostat - A Modern Xanthine Oxidase Inhibitor
First approved in 2009, Febuxostat an oral xanthine oxidase inhibitor that lowers uric acid without needing renal dose adjustments offers a tidy solution for patients who can’t tolerate allopurinol’s renal limitations.
- Dosing: 40mg once daily, titrated to 80mg or 120mg if needed.
- Renal safety: No dose reduction required down to eGFR 30mL/min/1.73m².
- Side‑effects: Liver‑function bumps, mild rash, occasional gout flare during initiation.
- Cardiovascular note: FDA boxed warning for patients with existing heart disease; discuss risk‑benefit.
Clinical trials (e.g., FEATHER) showed febuxostat achieving target urate in ~70% of patients with stage3 CKD, outperforming allopurinol at comparable doses.
Probenecid - The Urate‑Excreting Partner
Probenecid a uricosuric drug that increases renal excretion of uric acid works the opposite way: instead of blocking production, it helps the kidneys throw excess uric acid out.
- Dosing: 250mg twice daily, max 2g per day.
- Best for: Patients with under‑excreted uric acid and good kidney function (eGFR>50).
- Contra‑indications: History of kidney stones, severe CKD, or concurrent nephrotoxic drugs.
- Side‑effects: GI upset, rash, and rare hemolysis in G6PD‑deficient individuals.
Because probenecid relies on the kidneys, it’s often paired with a low dose of allopurinol or febuxostat when a single agent can’t hit the target.
Lesinurad - The Boosting Add‑on
Approved in 2015, Lesinurad a selective uric‑acid reabsorption inhibitor used in combination with a xanthine oxidase inhibitor adds extra uric‑acid clearance to patients already on allopurinol or febuxostat.
- Dosing: 200mg or 400mg once daily, taken with a xanthine oxidase inhibitor.
- Renal caution: Not for eGFR<30; monitor serum creatinine.
- Side‑effects: Acute kidney injury, especially if volume‑depleted.
Studies (e.g., CLEAR 1 & 2) demonstrated an extra 12-15% of patients reaching urate<120µmol/L when lesinurad was added to febuxostat.
Pegloticase - The Intravenous Rescue
For the toughest cases, Pegloticase a recombinant uric‑acid oxidase given IV that converts uric acid to allantoin is a biotech option used when oral drugs fail.
- Dosing: 8mg IV infusion every two weeks.
- Indication: Chronic refractory gout with urate>480µmol/L despite max oral therapy.
- Side‑effects: Infusion reactions, anti‑pegloticase antibody formation, rare anaphylaxis.
- Monitoring: Serum uric acid should drop below 120µmol/L within 24h of first infusion.
Real‑world data from US clinics show ~70% of patients achieve target urate within three months, but the need for IV visits limits widespread use.
Topiroxostat - The Asian Contender
While not yet FDA‑approved, Topiroxostat a potent xanthine oxidase inhibitor marketed in Japan and Europe offers another oral route with a favorable renal profile.
- Dosing: 50mg twice daily, titrated to 200mg.
- Renal safety: Minimal dose adjustment needed down to eGFR20mL/min/1.73m².
- Side‑effects: Mild liver‑enzyme elevation, GI upset.
- Evidence: Phase‑III studies in Japan report 71% target‑urate achievement, comparable to febuxostat.
If you’re in the UK and can access through a clinical trial or compounding pharmacy, topiroxostat might become a useful alternative in the near future.
How to Choose the Right Therapy
Picking the best medication isn’t a one‑size‑fits‑all decision. Consider these five practical criteria:
- Kidney function: eGFR<30mL/min pushes you toward febuxostat, topiroxostat, or low‑dose allopurinol with close monitoring.
- Cardiovascular risk: If you have heart failure or recent MI, weigh febuxostat’s boxed warning against allopurinol’s broader safety record.
- History of rash or hypersensitivity: Switch to a uricosuric (probenecid) or a newer xanthine oxidase inhibitor.
- Urate‑excretion capacity: A 24‑hour urine uric‑acid test can tell if a uricosuric will help.
- Patient preference & lifestyle: Oral daily pills are easier than bi‑weekly IV infusions; cost and NHS formulary status matter too.
Talk to your GP or rheumatologist about lab values, comorbidities, and how each drug fits your daily routine.
Quick Comparison Table
| Medication | Mechanism | Typical Dose | Renal Adjust. | Main Side‑effects | Approx. UK Cost* |
|---|---|---|---|---|---|
| Allopurinol | Xanthine oxidase inhibitor | 100‑600mg daily | Reduce dose if eGFR<30 | Rash, liver elevation, rare hypersensitivity | £4‑£8 per month |
| Febuxostat | Xanthine oxidase inhibitor | 40‑120mg daily | No adjustment down to eGFR30 | Liver enzymes, cardiovascular warning | £30‑£45 per month |
| Probenecid | Uricosuric - blocks renal reabsorption | 250‑500mg twice daily | Not for eGFR<50 | Kidney stones, GI upset | £12‑£20 per month |
| Lesinurad | URAT1 inhibitor (adds to XO‑inhibitor) | 200‑400mg daily | Avoid if eGFR<30 | Acute kidney injury, rash | £45‑£60 per month |
| Pegloticase | Uric‑acid oxidase (IV) | 8mg bi‑weekly infusion | Not limited by kidney function | Infusion reactions, antibodies | £1,200‑£1,500 per infusion |
| Topiroxostat | Xanthine oxidase inhibitor | 50‑200mg daily | Minimal adjustment | Liver enzyme rise, mild GI | £35‑£50 per month (off‑label) |
*Prices are indicative NHS pharmacy list prices (2025) and may vary by region.
Next Steps for Patients
1. Get baseline labs. Serum uric acid, eGFR, LFTs, and a 24‑hour urine uric‑acid test give a clear picture.
2. Discuss comorbidities. Heart disease, kidney disease, and medication list shape the safest option.
3. Trial a low dose. Start with the smallest effective dose of your chosen drug, then titrate every 2‑4 weeks.
4. Monitor closely. Check uric acid after 4 weeks; if you’re still >360µmol/L, adjust dose or add a second agent.
5. Stay proactive. Lifestyle tweaks-hydration, low‑purine diet, weight loss-boost any medication’s effectiveness.

Frequently Asked Questions
Can I switch from allopurinol to febuxostat without a washout period?
Yes. Because both are xanthine oxidase inhibitors, you can transition directly. Most clinicians stop allopurinol and start febuxostat the next day, monitoring uric acid for a week to avoid a flare.
Is probenecid safe if I have a history of kidney stones?
No. Probenecid increases uric‑acid excretion, which can raise stone‑forming risk. If you’ve had stones, a uricosuric is usually avoided.
What triggers allopurinol hypersensitivity syndrome?
High starting doses (≥300mg) in patients with renal impairment, plus concurrent drugs like azathioprine, raise the risk. Gradual dose titration and HLA‑B*58:01 screening in Asian populations lower the chance.
Do I need regular blood tests on pegloticase?
Yes. Check uric acid before each infusion and monitor liver enzymes and renal function monthly. If uric acid spikes above 360µmol/L, an antibody may have formed and the drug should be stopped.
Is topiroxostat available on the NHS?
Not yet. It’s licensed in Japan and some EU countries but hasn’t received UK market authorization. Patients may obtain it via clinical trials or private import.


13 Comments
Sumeet Kumar
When you have any degree of renal impairment, start Allopurinol at 50 mg daily and titrate very slowly – the kidneys can’t clear higher doses efficiently 😊. Keep an eye on serum creatinine and adjust the dose every 2–4 weeks based on labs. If you notice a rash, stop the drug immediately; hypersensitivity can progress quickly. For patients on warfarin, monitor INR more closely after the dose changes. Remember, the goal is to keep uric acid below 6 mg/dL, not to chase the highest possible dose.
Maribeth Cory
Febuxostat shines when you’re worried about the cardiovascular bells and whistles that come with allopurinol dose‑escalation. Studies show a modest increase in heart‑related adverse events in high‑risk patients, so weigh that against the renal safety benefit. If you’re on azathioprine, a slight reduction in allopurinol dose often does the trick, but keep the liver panel in check. Probenecid can be a good add‑on if you have decent kidney function and no history of stones. Ultimately, shared decision‑making with your rheumatologist will land you the right regimen.
andrea mascarenas
Allopurinol dose is based on eGFR. Reduce by 50% if eGFR is 30‑50. Below 30 mL/min you may need 100 mg or less. Watch for rash. No heavy punctuation here
Vince D
Allopurinol works fine for most people.
Camille Ramsey
Listen up folks, if you think you can just pop a high dose of allopurinol without checking your kidneys you are asking for trouble – it's not rocket science. The drug builds up and can cause a life‑threatening hypersensitivity rash that will have you in ICU faster than you can say “gout”. And don't even get me started on the interactions with warfarin – you might end up bleeding out if you aren't careful. Yeah, febuxostat looks shiny, but it comes with its own heart warnings, so don't just jump ship without a plan. Bottom line: respect the dosing guidelines or suffer the consequences.
Scott Swanson
Oh, because we all love a good drama lesson before breakfast, right? 🙄 If you actually read the prescribing info, you'd see the warnings are there for a reason, not just for drama queens. Maybe next time try a tone that doesn't scream “I’m yelling at the internet”.
Karen Gizelle
While brevity has its place, reducing complex pharmacotherapy to a single sentence risks oversimplification. Allopurinol's efficacy hinges on appropriate titration, renal monitoring, and patient adherence. Ignoring these nuances may lead to suboptimal urate control or adverse events. Therefore, a more thorough discussion is advisable for anyone starting therapy.
Stephanie Watkins
That clarification on febuxostat’s cardiovascular profile is helpful – many patients aren’t aware of that trade‑off. Also, the suggestion to monitor INR when adjusting allopurinol with warfarin is solid. Thanks for pulling together those practical tips.
Zachary Endres
Gout can feel like a punch to the toe, but remember you’re not alone in this battle. Whether you stick with Allopurinol, switch to Febuxostat, or add Probenecid, each path has its own set of checkpoints. Keep a diary of flare frequency and uric‑acid labs – the data will guide you better than guesswork. Talk openly with your doctor about side‑effects; they can tweak doses before things get out of hand. Celebrate the small victories, like a week without pain, and stay motivated.
Ashley Stauber
While the low‑and‑slow approach works for many, some patients argue that early aggressive dosing can achieve target levels faster. That perspective, however, overlooks the increased risk of hypersensitivity in vulnerable populations.
Amy Elder
Interesting read. The interactive selector could be a useful tool for patients to visualize options.
Will Esguerra
In the contemporary management of gout, the selection of urate‑lowering therapy must be predicated upon a comprehensive assessment of patient‑specific comorbidities, renal function, and pharmacodynamic interactions. Allopurinol, as a xanthine oxidase inhibitor, has long served as the cornerstone of therapy, yet its dose‑dependent nephrotoxic potential necessitates vigilant monitoring, particularly in individuals with compromised glomerular filtration rates. Febuxostat, while offering a more favorable renal safety profile, carries an FDA‑mandated warning regarding possible augmentation of cardiovascular events, a factor that must be weighed against its convenience of dosing. Probenecid, a uricosuric agent, exerts its effect by enhancing renal excretion of uric acid, but is contraindicated in patients with a history of nephrolithiasis or severe chronic kidney disease. Lesinurad, as an adjunctive therapy, amplifies urate clearance when combined with a xanthine oxidase inhibitor, yet its association with acute kidney injury mandates periodic assessment of serum creatinine and electrolytes. Pegloticase, reserved for refractory gout, presents logistical challenges due to its intravenous administration and the risk of infusion reactions, while topiroxostat remains primarily available outside of the United States. The clinician must also consider drug‑drug interactions; for instance, concurrent azathioprine may necessitate dose reduction of allopurinol to mitigate hematologic toxicity. Moreover, warfarin users require close INR monitoring when initiating or adjusting allopurinol dosages, due to potentiation of anticoagulant effects. Patient education remains paramount, as adherence to lifestyle modifications-such as reduced purine intake, alcohol moderation, and weight management-synergizes with pharmacotherapy to achieve target serum urate levels. Ultimately, a personalized algorithm that incorporates these variables can optimize therapeutic outcomes while minimizing adverse events. Future research should aim to delineate biomarkers that predict response to specific agents, thereby refining the precision of gout management.
Ben Poulson
The exposition provides an exhaustive overview, yet a few minor inaccuracies merit correction. Specifically, the claim that febuxostat’s cardiovascular warning applies uniformly to all patients overlooks the recent data suggesting a lower absolute risk in low‑risk cohorts. Additionally, the statement regarding topiroxostat’s unavailability in the United States should reference its ongoing clinical trials rather than imply permanent exclusion. Nevertheless, the systematic approach outlined aligns well with current guideline recommendations.