Anemia & Bone Health Risk Calculator
Assess Your Risk
Answer the following questions to determine your risk level for bone problems related to anemia. This tool helps identify potential connections between low blood counts and bone health issues.
Your Risk Assessment
Iron-deficiency anemia reduces oxygen delivery to bone marrow, slowing bone formation. Vitamin D deficiency impairs calcium absorption, weakening bones. Chronic inflammation from conditions like inflammatory bowel disease accelerates bone breakdown. Age increases risk as bone remodeling slows. Regular exercise supports bone strength.
When you hear the word anemia, you probably think of fatigue, pale skin, and shortness of breath. What if I told you that the condition can also weaken your bones and raise the risk of osteoporosis? In this article we’ll unpack how low red blood cell counts and poor iron status can sabotage bone strength, what the science says, and what practical steps you can take to protect both your blood and your skeleton.
What Is Anemia?
Anemia is a medical condition in which the blood lacks enough healthy red blood cells or sufficient hemoglobin to carry adequate oxygen to the body’s tissues. The most common cause is iron deficiency, but chronic disease, vitamin B12 deficiency, and genetic disorders also play a role. Typical symptoms include tiredness, dizziness, rapid heartbeat, and reduced exercise capacity.
Understanding Osteoporosis
Osteoporosis is a skeletal disorder marked by low bone mineral density (BMD) and structural deterioration of bone tissue, leading to increased fracture risk. The condition often develops silently; many people only discover it after a fracture from a minor fall. Post‑menopausal women and older adults are the most affected groups, but men and younger individuals with certain risk factors can develop it too.
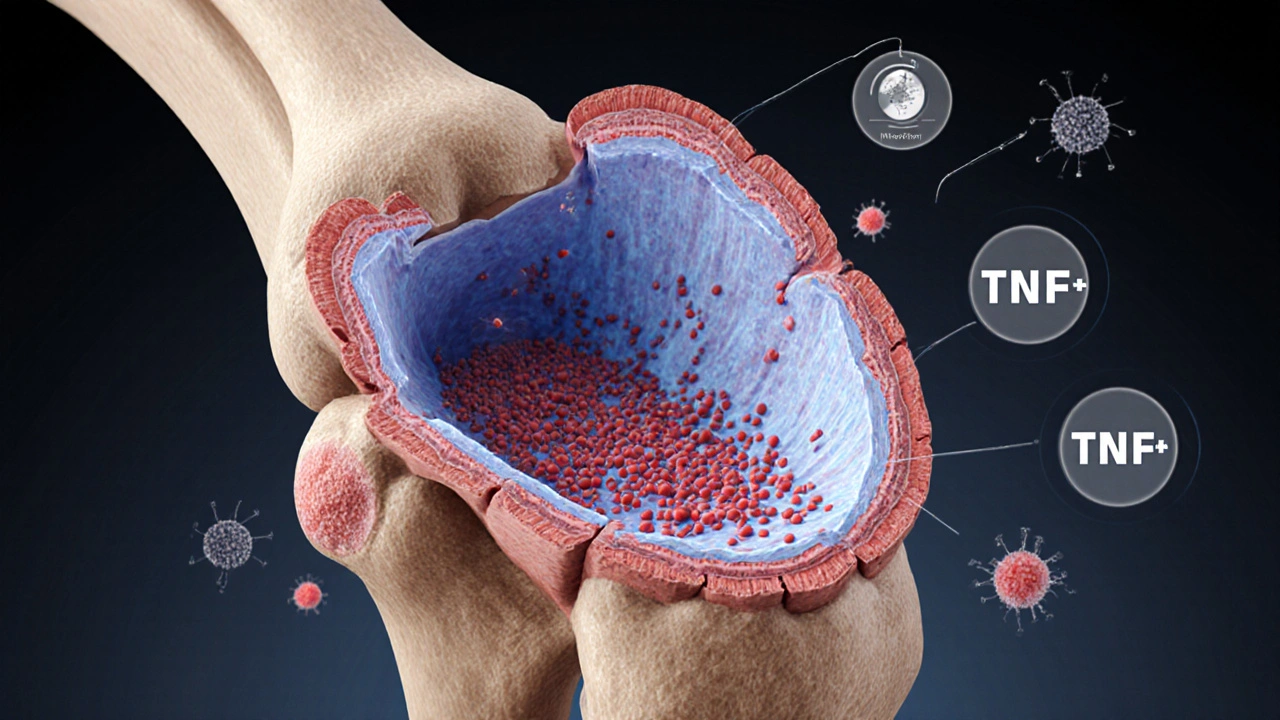
How Anemia Impacts Bone Remodeling
Bone is a living tissue that constantly remodels through a balance of osteoclast‑driven resorption and osteoblast‑driven formation. Several biological pathways link anemia to this balance:
- Oxygen delivery: Low Hemoglobin the protein in red blood cells that transports oxygen reduces oxygen tension in bone marrow, impairing osteoblast activity and favoring resorption.
- Erythropoietin (EPO) signaling: In response to anemia, kidneys release more Erythropoietin a hormone that stimulates red blood cell production. Elevated EPO has been shown in animal models to increase osteoclast formation, accelerating bone loss.
- Inflammatory cytokines: Iron‑deficiency anemia often coexists with chronic inflammation, raising levels of IL‑6 and TNF‑α-both potently stimulate bone‑resorbing cells.
- Nutrient competition: The body prioritizes iron for hemoglobin synthesis over calcium and vitamin D metabolism, potentially leading to lower serum calcium and reduced activation of vitamin D.
These mechanisms create a perfect storm where bone formation slows while breakdown speeds up, nudging a person toward osteoporotic changes.
Key Risk Factors Linking Anemia and Bone Loss
| Risk Factor | Effect on Blood | Effect on Bone |
|---|---|---|
| Iron‑deficiency | ↓ Hemoglobin, ↓ RBC count | ↓ Osteoblast activity, ↑ Resorption |
| Vitamin D deficiency | Impaired calcium absorption, may worsen anemia | ↓ Calcium deposition, weaker bone matrix |
| Chronic kidney disease | Reduced EPO production → anemia | Altered mineral balance, secondary hyperparathyroidism |
| Inflammatory bowel disease | Blood loss, malabsorption of iron | Inflammation‑driven osteoclast activation |
| Menopause | Hormonal changes may affect iron metabolism | ↓ Estrogen → ↑ Bone turnover |
Notice how many of these factors overlap with classic osteoporosis triggers-low calcium, vitamin D insufficiency, and chronic inflammation. That overlap explains why patients with persistent anemia often show early signs of reduced BMD on DXA scans.
Protecting Your Bones When You Have Anemia
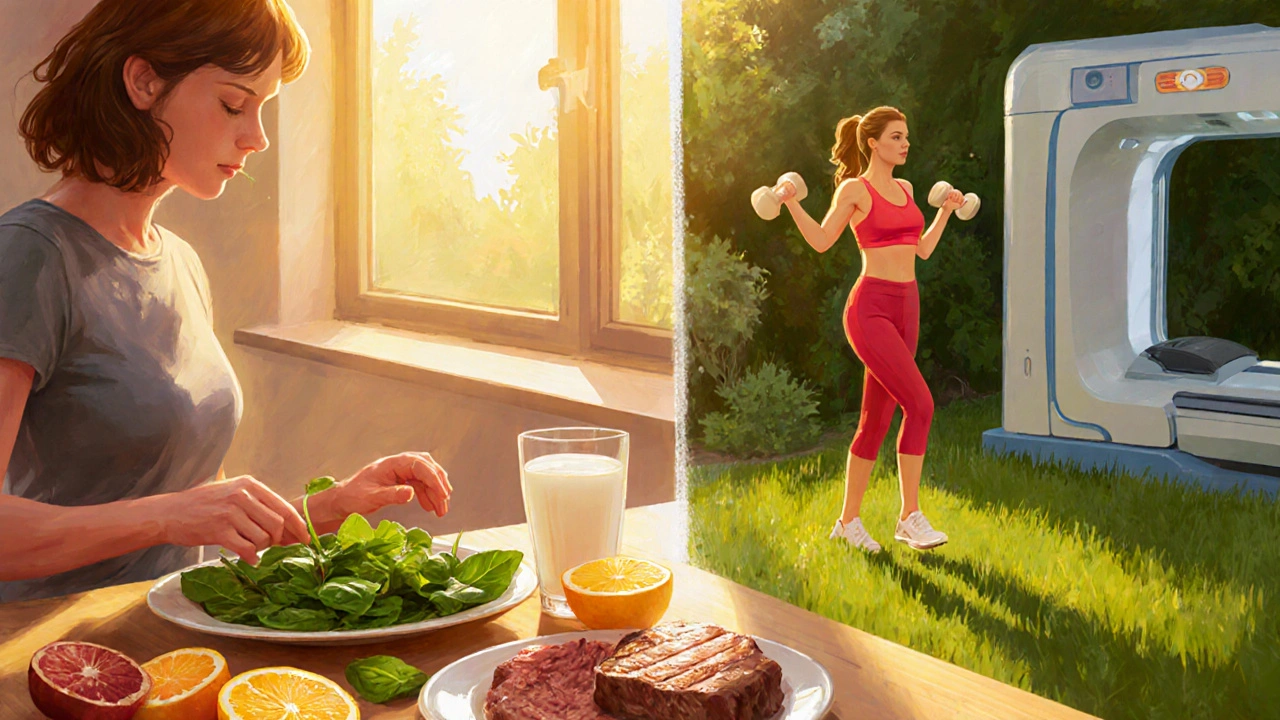
Addressing anemia can be a double win for bone health. Here’s a practical checklist you can follow:
- Identify the anemia type: Get a full blood count, serum ferritin, vitamin B12, folate, and in some cases, reticulocyte count. Pinpointing the cause guides targeted treatment.
- Replenish iron wisely: Oral ferrous sulfate (150mg elemental iron) is first‑line for iron‑deficiency anemia, but take it with vitamin C to boost absorption and avoid taking it with calcium-rich foods or antacids.
- Consider intravenous iron: If oral iron is poorly tolerated or you need rapid correction (e.g., before orthopedic surgery), IV iron formulations can normalize ferritin within weeks.
- Boost vitamin D and calcium: Aim for 800-1,000IU of vitamin D3 daily and 1,000-1,200mg of calcium from diet or supplements. These nutrients support both hemoglobin synthesis and bone matrix formation.
- Exercise for bone strength: Weight‑bearing activities-walking, jogging, resistance training-stimulate osteoblasts and improve circulation, which helps oxygen delivery to bone marrow.
- Manage underlying disease: Treat chronic kidney disease, inflammatory bowel disease, or hormonal disorders that contribute to both anemia and bone loss.
- Monitor bone density: If you’ve had anemia for more than six months, ask your doctor for a DXA scan. Early detection of low BMD can trigger anti‑resorptive therapy (bisphosphonates, denosumab) before a fracture occurs.
These steps create a feedback loop: healthier blood carries more oxygen, which fuels bone‑building cells, while improved bone health can reduce inflammation that often worsens anemia.
Key Takeaways
- Anemia, especially iron‑deficiency, reduces oxygen delivery to bone marrow, hindering bone formation.
- Elevated erythropoietin and inflammatory cytokines in anemia can accelerate bone resorption.
- Common risk factors-vitamin D shortage, chronic inflammation, menopause-link the two conditions.
- Treating anemia with iron, vitamin D, calcium, and disease‑specific therapy can improve bone mineral density.
- Regular bone density testing is advisable for anyone with persistent anemia over six months.
Frequently Asked Questions
Can mild anemia really affect my bones?
Yes. Even mild reductions in hemoglobin lower oxygen levels in the bone marrow, which can subtly impair osteoblast activity over time. Studies in middle‑aged adults show a 10‑15% higher odds of low BMD when hemoglobin drops below 12g/dL.
Is there a direct test that links anemia to bone loss?
There isn’t a single test, but clinicians often combine a full blood count, serum ferritin, vitamin D level, and a dual‑energy X‑ray absorptiometry (DXA) scan. Correlating low hemoglobin with reduced T‑scores helps confirm the connection.
Should I take iron supplements if I’m already on calcium?
Iron and calcium compete for absorption in the gut. It’s best to separate them by at least two hours-take iron with vitamin C in the morning and calcium with dinner.
Does treating anemia reverse osteoporosis?
Treating anemia can halt further bone loss and, in some cases, modestly improve BMD, especially when combined with calcium, vitamin D, and weight‑bearing exercise. Full reversal of established osteoporosis usually requires additional bone‑specific medication.
Are there dietary foods that support both blood and bone health?
Leafy greens (spinach, kale) provide iron and calcium; fatty fish and fortified dairy supply vitamin D; citrus fruits boost iron absorption. Combining these foods each day creates a nutrient profile that benefits both systems.

10 Comments
Meigan Chiu
I doubt anyone actually links mild anemia to osteoporosis.
Quiana Huff
Great breakdown! The interplay between erythropoietin signaling and osteoclast activation is a classic example of pathophysiological crosstalk. When you boost iron intake and trigger robust hematopoiesis, you also modulate the RANK‑L/OPG axis, which can tip the balance toward bone formation. Pair that with weight‑bearing exercise and you’ve got a multimodal strategy that hits both the hematologic and skeletal compartments. Keep this synergy in mind and you’ll see measurable improvements in BMD within months :)
William Nonnemacher
Another overhyped “connection” that pharma will exploit for profit.
Alex Ramos
Look, the data are clear: iron‑deficiency anemia reduces oxygen tension in the marrow, which impairs osteoblast function; simultaneously, elevated erythropoietin stimulates osteoclastogenesis, accelerating bone resorption; add chronic inflammation and you have a perfect storm for osteoporosis, especially in post‑menopausal women; therefore, clinicians should screen anemia patients for low BMD without hesitation; and patients must prioritize iron, vitamin D, and weight‑bearing exercise as a triple‑threat regimen!
Mita Son
Oh my god, you guys have no idea how this hidden link can silently wreck your skeleton! Imagine being tired all the time, thinking it’s just “normal” fatigue, while deep inside your marrow is starving for oxygen. That tiny drop in hemoglobin means your bone‑building cells are practically on a coffee break, and the osteoclasts are partying all night long. And don’t even get me started on the nasty cytokines-IL‑6 and TNF‑α are like little saboteurs, tearing down bone tissue while you’re busy scrolling through memes. If you’re over fifty and already dealing with menopause, the risk skyrockets like a fireworks show on the fourth of July. So, yes, iron‑deficiency isn’t just about pale skin; it’s a silent assassin of bone health, and you need to kick it to the curb before it cracks your hips!
Julien Martin
That’s a spot‑on summary! Addressing iron deficiency with proper supplementation, optimizing vitamin D status, and incorporating regular resistance training can indeed reverse some of the bone loss trends you highlighted. It’s also worth noting that monitoring ferritin and calcium levels concurrently helps fine‑tune the therapeutic plan. Keep spreading this info-early detection and a comprehensive approach are key to preserving skeletal integrity.
Jason Oeltjen
People should stop ignoring basic nutrition; it’s just common sense that a balanced diet prevents both anemia and weak bones.
Mark Vondrasek
Wow, another “breakthrough” article that tries to convince us that a simple blood test can predict your future fractures-how original. First, let’s acknowledge that the whole medical-industrial complex loves to sprinkle buzzwords like “crosstalk” and “cytokine storm” to sell you pills you don’t need. They’ll have you believing that a modest dip in hemoglobin magically turns your bones into a house of cards, when in reality most of us are dealing with lifestyle choices they conveniently ignore. Do you really think the pharma giants didn’t already know that iron supplements boost the sales of calcium tablets? It’s all part of the grand design to keep us hooked on a cocktail of vitamins, minerals, and overpriced DXA scans. And while we’re at it, let’s not forget the hidden agendas behind the “weight‑bearing exercise” recommendation-producers of gym equipment love a good hype. The article also conveniently skips over the socioeconomic factors that prevent many from accessing iron‑rich foods or safe places to exercise, as if everyone can just pop a pill and hit the gym at midnight. Meanwhile, the same researchers are busy publishing grant‑filled papers that cite each other in a never‑ending echo chamber. If you strip away the jargon, the core message is simple: improve your diet, get sunlight, and move more-nothing mystical. Yet they dress it up in clinical trial terminology to make it sound revolutionary, hoping we’ll feel guilty for not following the “prescribed protocol.” Personally, I’d rather trust my grandmother’s advice on bone broth and sunlight than a glossy infographic that claims anemia is the silent assassin of your skeleton. So, before you scramble to buy every supplement on the shelf, remember that the true power lies in common sense, not in a cascade of cytokines that only exist in a lab‑grown spreadsheet. In short, don’t let the hype distract you from the basics-eat well, stay active, and get your blood checked when you actually feel off, not because every article tells you to. If you keep questioning why the narrative feels so manufactured, you’re onto something the industry doesn’t want you to see. Bottom line: trust evidence, not marketing fluff, and your bones will thank you.
Joshua Agabu
That’s an entertaining take, but I think the basics you mentioned-diet, sunlight, exercise-still hold true for most people.
Lolita Rosa
Honestly, this whole debate feels like a circus, but if we’re all just trying to stay healthy, let’s stop the drama and follow the simple advice already laid out.