Hypertrophic Subaortic Stenosis Risk Calculator
This tool estimates the risk of sudden cardiac death based on MRI findings and clinical factors.
Quick Takeaways
- Cardiac MRI provides detailed tissue characterization that echo cannot match.
- Late gadolinium enhancement (LGE) on MRI predicts sudden cardiac death risk in hypertrophic subaortic stenosis.
- Cine MRI accurately measures left ventricular outflow tract (LVOT) gradients and septal thickness.
- Combining MRI findings with genetic testing refines treatment choices such as myectomy or septal ablation.
- Despite higher cost, MRI’s comprehensive data often prevents unnecessary invasive procedures.
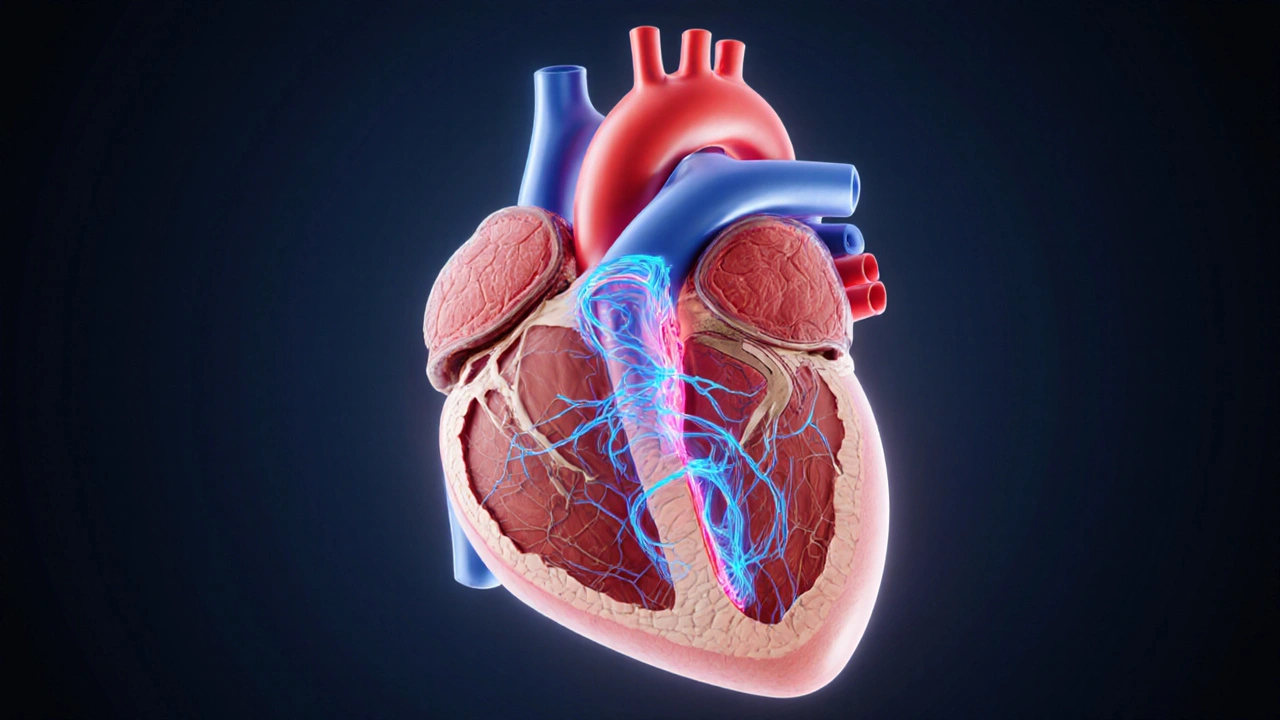
When it comes to visualizing the heart’s structure, Cardiac MRI is a non‑invasive imaging technique that provides high‑resolution, three‑dimensional views of myocardial tissue, blood flow, and functional dynamics. For patients with Hypertrophic Subaortic Stenosis (Hypertrophic Obstructive Cardiomyopathy), this level of detail can be the difference between a vague diagnosis and a life‑saving treatment plan.
Understanding Hypertrophic Subaortic Stenosis
Hypertrophic Subaortic Stenosis is a form of cardiomyopathy where the interventricular septum thickens abnormally, narrowing the Left Ventricular Outflow Tract (LVOT) and creating a dynamic obstruction. Most patients present with exertional dyspnea, chest pain, or syncope, but the disease can also be silent until a sudden cardiac death (SCD) event occurs.
The genetics are complex: over a dozen sarcomere gene mutations (e.g., MYH7, MYBPC3) have been linked to the condition. However, phenotype severity does not always mirror genotype, making imaging essential for risk stratification.
Why Imaging Matters
Traditional assessments-clinical exam, ECG, and transthoracic Echocardiography-provide a snapshot of ventricular size and flow gradients, but they fall short in three key areas:
- Detecting myocardial fibrosis, a predictor of arrhythmia.
- Quantifying exact septal thickness in atypical locations.
- Evaluating complex flow patterns that influence symptoms.
Cardiac MRI directly addresses each gap, delivering both anatomical and tissue‑level insight.
Core MRI Techniques for HSS
Modern cardiac MRI protocols typically include three pillars:
- Cine MRI: Steady‑state free precession (SSFP) sequences generate real‑time movies of the beating heart, allowing precise measurement of LVOT gradients and ejection fraction.
- Late Gadolinium Enhancement (LGE): After injecting a gadolinium‑based contrast agent, delayed images highlight areas of replacement fibrosis. In HSS, LGE often appears in the junctional zones between the septum and free wall.
- T1 Mapping & Extracellular Volume (ECV): Native T1 values and post‑contrast ECV quantify diffuse interstitial fibrosis, a subtle finding that echo can’t see.
Each sequence produces quantitative data that can be tracked over time, making MRI a powerful tool for monitoring disease progression.
How MRI Drives Evaluation and Diagnosis
When interpreting an MRI for HSS, radiologists look for four major markers:
- Septal Thickness: Values >15mm are considered diagnostic in the absence of other causes.
- LVOT Gradient: Phase‑contrast MRI quantifies peak systolic gradients; >30mmHg often correlates with symptomatic obstruction.
- Fibrosis Extent: Presence of LGE in >15% of left‑ventricular mass raises the SCD risk score.
- Myocardial Strain: Feature‑tracking on cine images reveals impaired longitudinal strain, an early sign of dysfunction.
These measurements feed directly into guideline‑based risk models, such as the 2020 ACC/AHA HCM risk calculator. Notably, the combination of a high LGE burden and a pathogenic sarcomere mutation often tips the scale toward implantable cardioverter‑defibrillator (ICD) placement.
Cardiac MRI vs. Echocardiography: A Head‑to‑Head Look
| Parameter | Cardiac MRI | Echocardiography |
|---|---|---|
| Spatial Resolution | 1‑2mm isotropic | 3‑5mm (dependent on acoustic window) |
| Fibrosis Detection | LGE & T1 mapping (quantitative) | Not assessable |
| LVOT Gradient Measurement | Phase‑contrast MRI (accurate, reproducible) | Doppler echo (operator‑dependent) |
| Assessment of Adjacent Structures | Full thoracic coverage (aorta, pulmonary veins) | Limited view |
| Availability & Cost | Limited to tertiary centers; higher cost | Widely available; lower cost |
Both modalities are complementary. Echo remains the first‑line tool for screening, while MRI is the decisive exam when therapeutic decisions hinge on fibrosis burden or ambiguous gradients.
Clinical Impact: From Risk Stratification to Treatment Choices
Integrating MRI findings into patient management follows a clear pathway:
- Identify High‑Risk Patients: LGE involving ≥15% of myocardium, extensive native T1 elevation, or a peak LVOT gradient >50mmHg flags patients for ICD consideration.
- Guide Surgical Interventions: Precise septal thickness maps help surgeons plan Septal Myectomy or percutaneous alcohol septal ablation, minimizing collateral damage.
- Tailor Pharmacologic Therapy: Patients with mild obstruction but marked fibrosis may benefit from beta‑blockers or disopyramide to reduce symptoms while monitoring for progression.
- Inform Family Screening: When MRI confirms a HSS phenotype, cascade genetic testing can be offered to first‑degree relatives, with MRI as a baseline surveillance tool.
In practice, a 45‑year‑old male with a septal thickness of 18mm, an LVOT gradient of 38mmHg, and 12% LGE might avoid ICD implantation today but would be re‑evaluated annually. Conversely, a similar patient with 25% LGE would be counseled for ICD placement despite a lower gradient.
Practical Considerations: Protocols, Contra‑indications, and Costs
Standard HSS MRI protocols include:
- Localizer and breath‑hold cine SSFP (3‑short‑axis, 2‑long‑axis planes).
- Phase‑contrast flow sequence across the LVOT.
- Pre‑contrast T1 mapping (MOLLI or SASHA).
- Gadolinium bolus (0.1mmol/kg) followed by LGE imaging 10‑15minutes later.
- Post‑contrast T1 mapping for ECV calculation.
Contra‑indications are few: implanted ferromagnetic devices, severe claustrophobia, or renal impairment (eGFR<30mL/min/1.73m²) that precludes gadolinium use. Newer macrocyclic agents reduce the risk of nephrogenic systemic fibrosis, allowing many patients with moderate renal dysfunction to safely undergo LGE.
Cost varies by geography. In Australia, a full cardiac MRI package averages AUD$1,200-$1,500, often covered by Medicare for high‑risk cardiomyopathy cases. The higher upfront expense is balanced by reduced downstream costs from avoided unnecessary surgeries or emergency events.
Future Directions: 4D Flow, AI‑Assisted Quantification, and Beyond
Emerging 4‑dimensional flow MRI captures the entire velocity field within the LVOT, providing insights into vortex formation that may explain symptom variability. Early studies suggest that certain vortex patterns correlate with higher obstruction severity.
Artificial‑intelligence algorithms are now being trained on thousands of HSS MRI datasets to automatically segment the myocardium, quantify LGE burden, and predict SCD risk with accuracy comparable to expert readers. As these tools mature, turnaround time could shrink from hours to minutes, making MRI a point‑of‑care decision aid.
Frequently Asked Questions
Is cardiac MRI safe for people with pacemakers?
Most modern pacemakers are MRI‑conditional, meaning they can safely undergo a scan under specific protocols. Always inform the imaging team about any implanted device so they can verify compatibility before the exam.
How often should a patient with hypertrophic subaortic stenosis get a cardiac MRI?
If the initial MRI shows no significant fibrosis and symptoms are stable, a repeat scan every 2-3years is typical. Presence of LGE or a rising LVOT gradient may prompt annual imaging.
Can cardiac MRI replace echocardiography for diagnosis?
No. Echo remains the first‑line tool because it’s quick, inexpensive, and excellent for real‑time hemodynamics. MRI is used when echo results are inconclusive or when detailed tissue characterization is needed.
What does a positive LGE finding mean for a patient?
LGE indicates replacement fibrosis, which is associated with a higher risk of ventricular arrhythmias and sudden cardiac death. The amount of LGE helps clinicians decide whether an ICD is warranted.
Are there any risks associated with gadolinium contrast?
Gadolinium is generally safe, but patients with severe kidney disease risk nephrogenic systemic fibrosis. Using macrocyclic agents and screening renal function mitigates this risk.


13 Comments
JOJO Yang
The very act of ignoring the MRI data is a betrayal of our duty to patients, a scandal that reeks of negligence! We cannot stand by as clinicians defiantly dismiss the stark evidence of fibrosis-its presence alone should trigger an ethical alarm. Those who rely solely on echo while dismissing LGE are, quite frankly, betraying the Hippocratic Oath-its a moral failing of epic proportions. If we let cost or convenience dictate care, we are complicit in preventable deaths. The community must rally, demand comprehensive MRI evaluation, and shame those who shirk responsibility.
Warren Workman
While the post extols CMR as the gold standard, one must interrogate the underlying signal‑to‑noise ratio (SNR) limitations and off‑resonance artifacts that can confound LGE quantification. Moreover, the reliance on a binary ≥15% LGE threshold neglects the continuum of extracellular volume fraction (ECV) metrics, which arguably provide a more granular risk stratification. The statement that phase‑contrast MRI yields "accurate, reproducible" LVOT gradients overlooks the intrinsic phase‑wrap errors in turbulent flow regimes, necessitating parallel imaging corrections. In essence, the algorithmic risk calculator simplifies a multivariate physiological tableau into an over‑engineered decision tree, which may inadvertently propagate systematic bias.
Kate Babasa
Indeed, the integration of CMR metrics-septal thickness, LVOT gradient, LGE percentage-into a unified risk matrix represents a commendable advance; however, clinicians must remain vigilant, ensuring that each parameter is interpreted within its hemodynamic context, lest we fall prey to reductionist pitfalls. Furthermore, the table contrasting MRI with echocardiography succinctly highlights the trade‑offs, yet the nuanced interplay of spatial resolution versus accessibility warrants a balanced discourse; after all, the choice of modality should be patient‑centric, not merely institution‑driven.
king singh
I think the data looks solid.
Adam Martin
Wow, another glittering piece of literature that promises to solve the enigma of hypertrophic subaortic stenosis with a few clicks.
The author neatly bundles septal thickness, LVOT gradients, and the ever‑mysterious LGE percentage into a tidy calculator, as if the complexities of myocardial architecture could be distilled into a spreadsheet.
Yet the underlying pathophysiology is anything but tidy, involving intricate sarcomeric mutations, microvascular ischemia, and phenotypic variability that no algorithm can fully capture.
One must appreciate that a 15% LGE cutoff, while convenient, stems from retrospective cohort analyses fraught with selection bias.
Moreover, the phase‑contrast MRI technique, although praised for its reproducibility, remains susceptible to aliasing artifacts when the LVOT jet exceeds the velocity encoding limit.
In clinical practice, the decision to implant an ICD often hinges on a constellation of factors-family history, syncope episodes, and patient preferences-that the calculator conveniently ignores.
The table comparing MRI and echo is a useful visual, but it oversimplifies the reality where echo operators with decades of experience can extract Doppler gradients with uncanny precision, sometimes surpassing MRI in dynamic assessments.
Conversely, MRI offers the unparalleled advantage of tissue characterization, revealing fibrosis that may be the silent harbinger of sudden cardiac death.
Nevertheless, the cost and limited availability of high‑field scanners pose a barrier, especially in community hospitals where echo remains the workhorse.
From a research standpoint, the inclusion of T1 mapping and extracellular volume calculations would elevate the risk model beyond binary LGE thresholds, providing a continuum of risk.
The author’s recommendation to re‑evaluate patients annually is prudent, yet the logistical burden of repeat MRI, gadolinium exposure, and patient compliance cannot be dismissed lightly.
In my experience, a multidisciplinary heart team-cardiologists, radiologists, genetic counselors-delivers the most nuanced management plan, something a solitary calculator cannot replicate.
That said, the tool does serve an educational purpose, prompting clinicians to consider metrics they might otherwise overlook.
If we embrace it as an adjunct rather than an oracle, it can augment shared decision‑making without us blindly surrendering to its outputs.
Ultimately, technology should empower, not replace, the physician’s judgment, and this risk calculator walks the fine line between helpful guide and overzealous babysitter.
Ryan Torres
Don't be fooled by the glossy MRI hype-big pharma and device manufacturers have a vested interest in inflating the LGE scare to sell more ICDs 😒. Every time you see a “high‑risk” label, ask who profits from the downstream procedures. The data is often cherry‑picked, and the so‑called ‘gold standard’ is just another revenue stream for imaging companies 🏥💰. Stay skeptical.
shashi Shekhar
Sure, let’s throw another expensive scan at every HCM patient and hope the numbers magically solve everything. Meanwhile, the real issue-access to basic care-is swept under the rug. Classic.
Marcia Bailey
Great analysis, Adam! Your points about multidisciplinary teams really hit home. For anyone wrestling with interpreting LGE, remember that quantitative T1 mapping can provide a more objective measure of fibrosis-try incorporating native T1 values into your assessment. Also, scheduling follow‑up MRIs every 12–18 months strikes a balance between vigilance and patient burden. Keep the conversation going! :)
melissa hird
It is truly astounding how the literature continues to champion ever‑more sophisticated imaging modalities while the underlying therapeutic conundrums remain unresolved. One might suggest that the relentless pursuit of higher resolution simply masks the fact that, in many instances, clinical outcomes have not markedly improved. Nevertheless, the dedication to technological advancement is, without doubt, admirable.
Mark Conner
Look, folks, American cardiology has always been on the cutting edge. We’ve got the best MRI tech, the sharpest minds, and we don’t settle for anything less than top‑notch care. If you’re in the US, you’re already ahead of the game.
Charu Gupta
While the discussion aptly highlights the merits of cardiac MRI, it is imperative to maintain grammatical precision in our discourse. For instance, the phrase “its a moral failing” should be rendered as “it’s a moral failing.” Additionally, the consistent use of the Oxford comma would enhance clarity. 📚
Abraham Gayah
Oh dear, yet another self‑appointed savior of cardiac imaging arrives, wielding buzzwords like a magician with a wand. The drama of the “risk calculator” is as overblown as a Hollywood sequel-full of sparkle, void of substance. Let’s not pretend this is the revolution we’ve been waiting for.
rajendra kanoujiya
Actually, the whole emphasis on MRI risk stratification is misguided; clinical judgment based on symptomatology still outperforms any algorithm.