When you're on a combination of NTI drugs, even a small change in dosage can be dangerous. These aren't ordinary medications. They're the kind where the line between healing and harm is razor-thin. Think warfarin, lithium, or levothyroxine - each one requires careful monitoring. Now imagine taking two of them together in a single pill. That’s combination NTI therapy. It’s used in serious conditions like advanced heart disease, certain cancers, or drug-resistant infections. But here’s the problem: almost no generic versions exist. And when they do, the risks go up - not down.
What Makes NTI Drugs So Tricky?
NTI stands for Narrow Therapeutic Index. That means the difference between a dose that works and one that causes harm is tiny. For most drugs, your body can handle some variation in strength. Not with NTI drugs. A 10% change in blood levels can mean the difference between controlling your condition and ending up in the hospital. The FDA defines them by five key traits: minimal safety margin, risk of life-threatening side effects, need for regular blood tests, low variability within the same person, and frequent small dose tweaks. Drugs like digoxin, phenytoin, and carbamazepine fall into this category. They’re powerful. They’re precise. And they’re unforgiving.
Why Combination NTI Drugs Are Rare - Even in Brand Form
Combination NTI therapy isn’t common because it’s hard to manage. But when it’s used, it’s usually because monotherapy isn’t enough. In tuberculosis, for example, isoniazid (an NTI drug) is paired with rifampin to prevent resistance. In oncology, methotrexate is combined with other targeted agents to kill cancer cells more effectively. But these combinations are almost always given as separate pills. Why? Because putting two NTI drugs into one tablet creates a scientific nightmare. Each drug has its own absorption rate, metabolism path, and clearance time. Even if both are perfectly bioequivalent on their own, together they can behave unpredictably. The FDA’s own data shows that only 12.6% of combination regimens involving NTI drugs have any generic version available - compared to 87.4% for single NTI drugs.
The Bioequivalence Wall
Generic drugs must prove they’re bioequivalent to the brand. For most drugs, that means the active ingredient must hit the bloodstream within 80% to 125% of the brand’s levels. For NTI drugs, that standard got tightened in 2014: 90% to 111% for peak concentration (Cmax) and 90% to 112% for total exposure (AUC). But when you combine two NTI drugs? The math gets worse. If each drug has a 22% allowed variation window, together that’s nearly 44% total variation - enough to cause serious harm. In 2023, the FDA proposed even stricter standards for combination NTI products: 90% to 107.69% for Cmax and 90% to 110% for AUC. That’s tighter than most manufacturers can reliably hit. No company has yet submitted a fixed-dose combination of two NTI drugs for approval in the U.S. Not one.

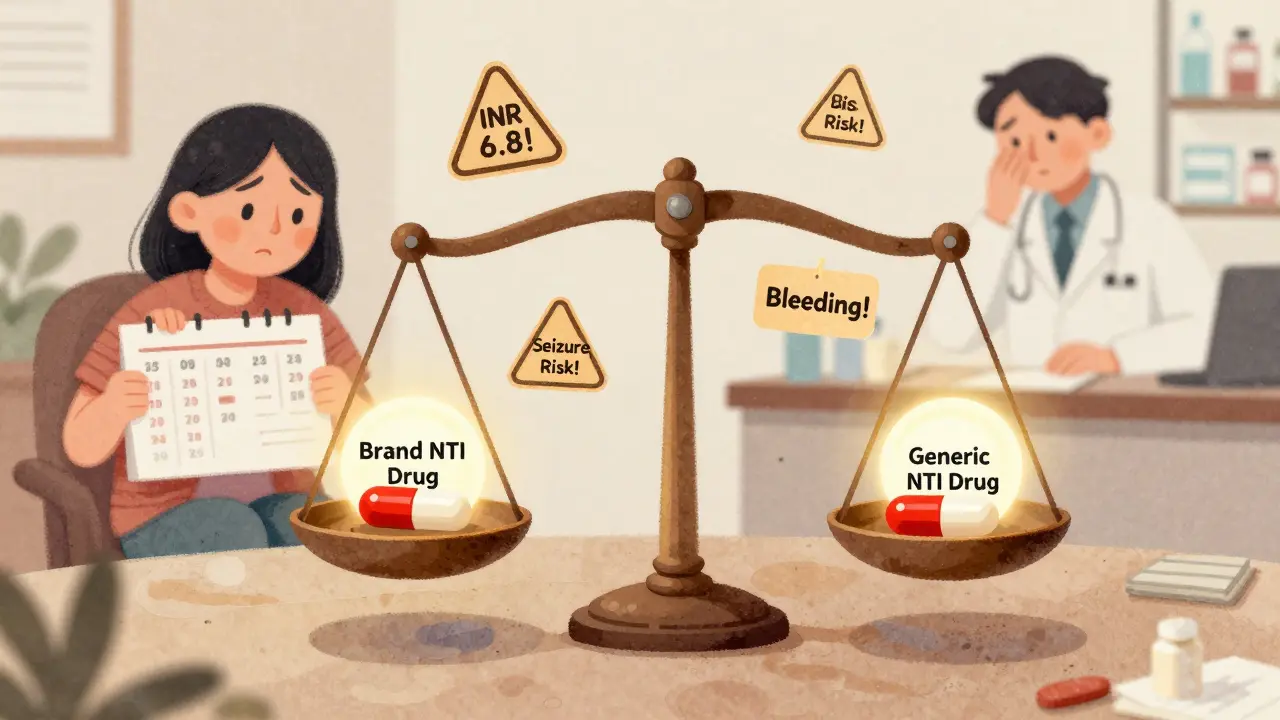
What Happens When Generics Are Used Anyway?
Even when a combination isn’t officially available as a single pill, patients often get one NTI drug as a generic and the other as brand. That’s where things get dangerous. A 2020 JAMA Internal Medicine study found that patients on combination therapy with even one NTI drug had a 27% higher chance of adverse events after generic substitution - compared to just 8% for non-NTI combinations. One patient on warfarin and amiodarone (both NTI drugs) reported his INR shot from 2.5 to 6.8 in three days after switching to generic warfarin. He ended up hospitalized. That’s not rare. A 2023 survey of 856 pharmacists found 78.3% had seen treatment failure after switching to generics in NTI combinations. Over 40% reported serious adverse events - bleeding, seizures, organ damage. The American Society of Health-System Pharmacists (ASHP) says automatic substitution of NTI drugs in combinations is an “unacceptable risk.”
Why Europe Seems to Be Doing Better
Some people point to Europe as proof it can work. Levothyroxine combinations with selenium or vitamin D have been used safely there since 2015, with adverse event rates under 2%. But there’s a catch: European regulators require individualized dosing and strict monitoring. Patients aren’t just handed a pill and told to go. They’re tracked closely with blood tests every few weeks. In the U.S., that level of oversight is rare outside major hospitals. Most patients get their meds from community pharmacies where pharmacists don’t have time to track INR levels or thyroid function daily. The difference isn’t in the drugs - it’s in the system. What works in a tightly managed German clinic doesn’t scale to a busy pharmacy in rural Texas.
The Cost of Monitoring
Managing combination NTI therapy isn’t cheap. Patients need frequent blood tests - sometimes every week at first. Annual monitoring costs range from $1,200 to $2,500 per person. That’s three to six times more than for non-NTI combinations. Most insurance plans cover the tests, but copays add up. And it’s not just money. It’s time. It takes 6 to 8 weeks to stabilize a patient on a combination NTI regimen. During that time, they might need three or four dose changes. That’s a lot of doctor visits, lab trips, and anxiety. For patients on fixed incomes, that’s a barrier. For providers, it’s a burden. Only 12 of the top 50 U.S. academic medical centers have dedicated NTI combination clinics. Most don’t have the staff or resources.

Who’s Pushing for Change - and Who’s Against It
Generic manufacturers like Teva and Sandoz argue that modern manufacturing can meet the tight standards. They point to advances in tablet compression, coating technology, and quality control. But critics say it’s not about the pills - it’s about the biology. Dr. Donald Berry, a biostatistician at MD Anderson, wrote in Nature Reviews Drug Discovery that even the tightened 90-111% window still allows too much variation when two NTI drugs are combined. “You’re multiplying uncertainty,” he said. Meanwhile, former FDA director Dr. Janet Woodcock admitted in 2022 that “combination products containing NTI drugs present even greater scientific challenges.” The FDA is now testing a pilot program using pharmacometric modeling to predict real-world outcomes instead of just blood levels. That could be a breakthrough - but it’s years away.
The Real Gap Isn’t Technology - It’s Trust
The biggest problem isn’t whether we can make these generics. It’s whether we can trust them. Patients who’ve been stable on brand-name drugs for years don’t want to risk a switch. One Reddit user wrote: “I’ve been on Synthroid and lithium for 12 years. My doctor won’t let me touch generics. He says if it ain’t broke, don’t fix it.” And he’s right. For many, the fear of instability outweighs the savings. A 2022 Drugs.com survey of 1,247 patients on NTI combinations showed 63.4% had adverse effects after switching to generics. Only 15% reported no issues - and most of those were on levothyroxine combinations with non-NTI supplements. The rest? They’re stuck. Either pay more for brand drugs or risk their health.
What Can Be Done?
Until better science and stricter regulations catch up, here’s what works: First, never switch NTI drugs - even one - without talking to your doctor. Second, ask if your pharmacy can keep you on the same brand. Many will, if you request it. Third, if you’re on a combination, insist on regular blood tests. Don’t wait for your next appointment. Fourth, document everything: dose changes, symptoms, lab results. Fifth, push your provider to join a specialized clinic if one exists nearby. There’s no magic solution yet. But awareness saves lives. The system isn’t designed for these complex cases. Until it is, patients and providers have to be their own safety net.
What are NTI drugs?
NTI drugs, or Narrow Therapeutic Index drugs, are medications where the difference between an effective dose and a toxic dose is very small. Examples include warfarin, lithium, levothyroxine, digoxin, and phenytoin. Even minor changes in blood levels can lead to treatment failure or serious side effects, so they require careful monitoring and precise dosing.
Why are there so few generic combination NTI drugs?
Combination NTI drugs are extremely hard to make as generics because each component has its own absorption and metabolism profile. When two NTI drugs are combined, even small variations in either one can multiply the risk of toxicity or failure. Current bioequivalence standards - even the tightened ones - don’t guarantee safety when multiple narrow-window drugs are mixed. No fixed-dose combination of two NTI drugs has been approved in the U.S. due to these scientific and regulatory barriers.
Is it safe to switch from brand to generic for a single NTI drug?
It can be, but only under close supervision. Studies show 18.7% of patients on warfarin experienced unstable INR levels after switching to generic versions. For drugs like levothyroxine, some patients do fine - but others don’t. Always consult your doctor before switching. If you do switch, get blood tests within 4-6 weeks to confirm levels are still in range.
What should I do if my pharmacy switches my NTI medication without telling me?
Ask for the original brand immediately. Under federal law, pharmacists can substitute generics only if the prescriber hasn’t marked "dispense as written" or if you’ve given consent. If you’re on an NTI drug, you have the right to refuse substitution. Keep a list of your medications and their brands. If you notice new symptoms - like fatigue, dizziness, or irregular heartbeat - contact your doctor right away.
Are there any NTI combination drugs available as generics anywhere?
There are no FDA-approved fixed-dose combinations of two NTI drugs in the U.S. In Europe, some combinations like levothyroxine with selenium or vitamin D are available, but they’re used under strict monitoring protocols. Even there, they’re not common. Most combination NTI therapies are still given as separate pills to allow individual dose adjustments.
How much does monitoring cost for combination NTI therapy?
Annual monitoring costs for combination NTI therapy average $1,200 to $2,500 per patient, compared to $400-$800 for non-NTI combinations. This includes frequent blood tests (INR, TSH, drug levels), doctor visits, and potential lab fees. Insurance often covers most of it, but copays and out-of-pocket costs can still add up quickly.
What’s being done to fix this problem?
The FDA is testing a new pilot program using pharmacometric modeling to predict how combination NTI drugs behave in real patients, instead of relying only on blood concentration tests. This could lead to better approval standards by 2026. Meanwhile, the EMA and other global agencies are tightening their own bioequivalence rules. But progress is slow. Until then, the safest approach is to avoid substitution and stick with proven regimens.

12 Comments
Radhika M
My mom’s on warfarin and levothyroxine. She switched to generics once and ended up in the ER with a bleeding ulcer. Now we pay extra for brand names. Worth every penny. Don’t risk it.
Philippa Skiadopoulou
The regulatory framework for NTI combinations remains fundamentally inadequate. Bioequivalence thresholds, even when tightened, fail to account for pharmacodynamic interactions. The FDA’s current model is statistically insufficient for clinical safety.
Pawan Chaudhary
Hey, I know this sounds scary but hear me out - there’s hope. My cousin’s a pharmacist in Bangalore and he’s seeing better generic stability now with new tech. It’s not perfect but progress is happening. Don’t give up.
Jonathan Morris
Let’s be real - this isn’t about science. It’s about Big Pharma protecting profits. The FDA’s ‘tightened standards’? A smokescreen. They’ve known for decades that combination NTI drugs can be made safe. But if generics were allowed, shareholders would lose billions. The real danger isn’t the meds - it’s the system.
Linda Caldwell
YOU ARE NOT ALONE. I was terrified too until I found my NTI clinic. They monitor me every two weeks. I pay more but I’m alive. If you’re reading this - reach out. Find your tribe. We got you.
Anna Giakoumakatou
Oh, so now we’re supposed to trust the same FDA that approved Vioxx and OxyContin? How quaint. The real tragedy isn’t the lack of generics - it’s that we still believe regulators care about patients more than liability waivers.
CAROL MUTISO
It’s wild how we treat people like lab rats when it comes to NTI drugs. We’ll let you switch generics but demand you track your INR like a scientist. Meanwhile, your insurance won’t cover the time off work or the Uber to the lab. The system doesn’t just fail you - it monetizes your fear. And somehow, we call this healthcare.
Jessica Salgado
I just found out my dad switched to generic carbamazepine last year and never told me. He’s had tremors and memory lapses since. I’m so angry. Why didn’t anyone warn us? This isn’t just about cost - it’s about silence.
amanda s
Europe does it better? Please. We’re the most advanced medical system on the planet. If other countries can’t handle NTI generics, that’s their problem. Stop comparing us to Germany. We don’t need their nanny-state policies.
Kent Peterson
Wait - so you’re saying that if you combine two drugs that each have a 10% variation window, you get a 20% total variation? That’s basic math. But the FDA’s 90–107.69% Cmax? That’s not tighter - it’s impossible. No one’s submitting because no one’s stupid enough to try. This whole thing is a scam.
Josh Potter
bro i just switched my levothyroxine to generic and i feel 10x better?? idk y everyone’s panicking. maybe it’s not the drug, maybe it’s the fear??
Jane Wei
I’m a nurse. I’ve seen this play out a hundred times. The pharmacy switches the generic, the patient gets dizzy, calls the clinic, and the doctor says ‘try the brand again.’ We’re just patching holes in a sinking ship.