For most people, the biggest surprise about generic drugs isn’t that they work-it’s how much money they save. You walk into the pharmacy, hand over your prescription, and expect to pay $50, $100, even $200 for a month’s supply. But instead, you’re handed a small bottle with a sticker that says generic and a price tag of under $10. That’s not a trick. It’s the system working exactly as it was designed to.
What Exactly Is a Generic Drug?
A generic drug isn’t a copy. It’s not a knockoff. It’s the exact same medicine as the brand-name version, just without the marketing budget. The FDA requires generics to have the same active ingredient, strength, dosage form, and route of administration as the original. They must also be bioequivalent-meaning they work in your body the same way, at the same rate, and with the same effect. There’s no difference in how they treat high blood pressure, diabetes, or depression. The only real difference? Price.The Real Cost Difference: Numbers That Speak Louder Than Ads
In 2024, the average out-of-pocket cost for a generic prescription was $6.95. For the same medicine in brand-name form? $28.69. That’s more than four times higher. For uninsured patients, the gap is even wider. Brand-name drugs jumped to $130.18 per prescription since 2019, while generic prices dropped by 6% over the same period. That’s not inflation. That’s a system where one side is being held hostage while the other keeps getting cheaper. The numbers get even more striking when you look at the whole system. In the U.S., 90% of all prescriptions filled in 2024 were for generic drugs. Yet those same generics made up only 12% of total prescription drug spending. Meanwhile, brand-name drugs-just 10% of prescriptions-accounted for 88% of the money spent. That’s the 90/12 paradox: most people take generics, but most of the money goes to brands. Since 2019, the U.S. has saved $445 billion just from using generic and biosimilar drugs. That’s not hypothetical. That’s real cash taken out of the system. Over the past decade, generic and biosimilar drugs saved Americans $3.4 trillion. Think about that: $3.4 trillion. That’s more than the entire annual GDP of Canada. And it all came from pills that cost pennies instead of dollars.How Do Generics Stay So Cheap?
The answer lies in the Hatch-Waxman Act of 1984. Before this law, generic manufacturers had to run the same expensive clinical trials as the original drug maker. That made generics impossible to produce at scale. Hatch-Waxman changed that. It created a shortcut: if a company could prove their version was bioequivalent to the brand, they didn’t need to repeat years of human trials. They just had to show the same chemistry, the same absorption rate, the same effect. That cut development costs by 80-90%. Once a patent expires, multiple generic companies can enter the market. Competition kicks in. One company lowers the price. Another drops it even more. Within months, the same pill that cost $100 as a brand can be $2 as a generic. And because the FDA requires every generic to meet the same standards, you’re not getting a weaker version-you’re getting the same medicine at a fraction of the cost.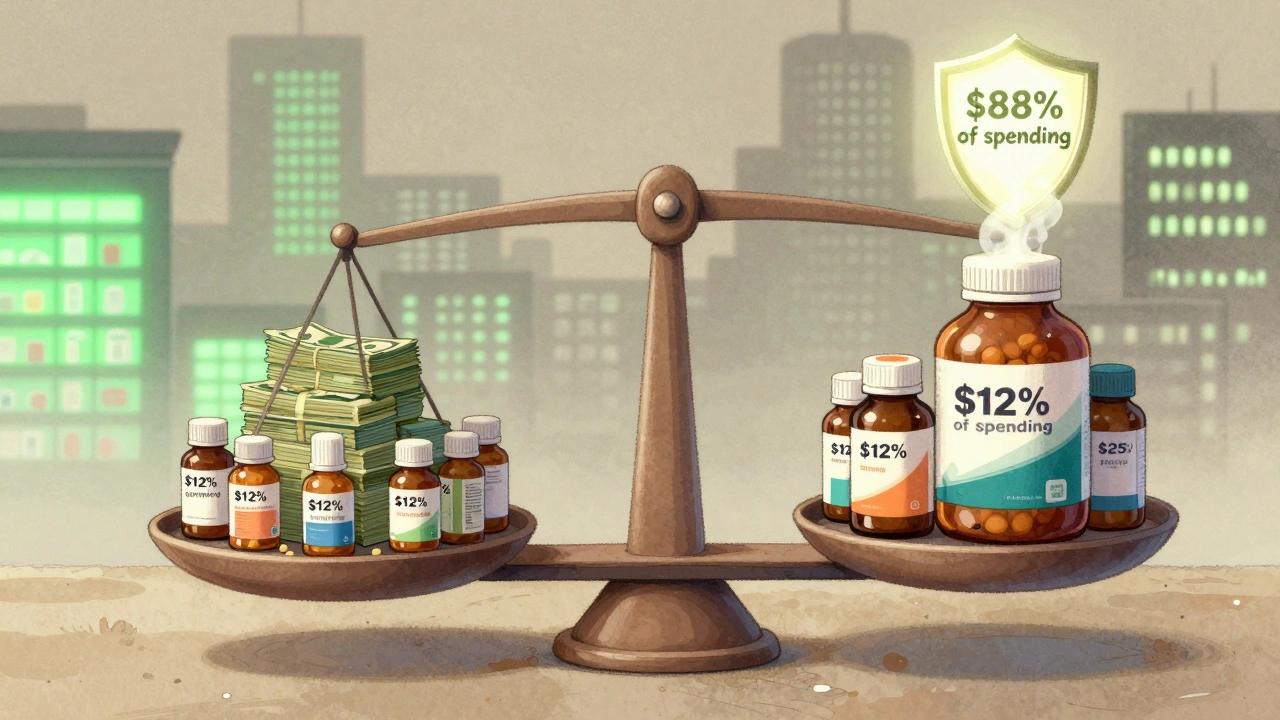
Biosimilars: The Next Wave of Savings
Biosimilars are the generic version of biologic drugs-complex medicines made from living cells, like those used for cancer, rheumatoid arthritis, and Crohn’s disease. They’re harder to copy than regular pills, which is why they took longer to arrive. But now they’re here, and they’re saving billions. Since their introduction, biosimilars have saved the U.S. healthcare system $56.2 billion. In 2024 alone, they saved $20.2 billion. One example: Stelara, a drug for psoriasis and Crohn’s, had a list price of over $6,000 per dose. When nine biosimilar versions hit the market in mid-2025, prices dropped by up to 90%. Suddenly, a treatment that was out of reach for many became affordable. Oncology biosimilars have cut the growth rate of cancer drug spending in half since 2019. In 2020, they saved $18 billion on cancer medicines alone. And yet, they still make up less than 30% of the market in most cases. That means there’s still billions more to save-if we let them in.Why Aren’t More People Using Generics?
If generics are so cheap and just as effective, why do some people still pay full price for brand names? The answer isn’t about quality. It’s about control. Big pharma doesn’t want generics to win. So they’ve built a system to delay them. One tactic is called “patent thickets.” Instead of filing one patent, companies file dozens-sometimes over 75-on the same drug. These cover everything from the pill’s shape to the coating to the way it’s manufactured. Even after the main patent expires, these secondary patents can block generics for years. One drug had its monopoly extended from 2016 to 2034 this way. Another trick is “product hopping.” A company slightly changes the drug-say, from a pill to a capsule-and pushes doctors to switch patients over. Then they file a new patent on the new version. The original patent expires, but patients are already locked into the new, expensive version. No generics can enter until that new patent runs out. These practices cost consumers nearly $12 billion a year, according to Blue Cross Blue Shield. About $3 billion of that is paid directly by patients.What’s Being Done to Fix It?
There’s growing pressure to break these monopolies. In early 2025, two bipartisan bills advanced in Congress: the Affordable Prescriptions for Patients Act, which targets patent thickets, and the Drug Competition Enhancement Act, which bans product hopping. If passed, they could save $2.9 billion over ten years. Pharmacy benefit managers (PBMs)-the middlemen who negotiate drug prices for insurers-are already pushing hard for generics. As of January 2025, 87% of commercial health plans require pharmacists to substitute generics when available. Medicare and Medicaid programs have similar rules. In hospitals and large health systems like Kaiser Permanente, switching to generics cut pharmacy costs by 25-35% within 18 months. The FDA approved 745 generic drugs in 2024-the highest number in over a decade. And with major drugs like Entresto, Tradjenta, and Opsumit losing patent protection in late 2025, we’re looking at $8.6 billion in brand sales about to be disrupted by generics.
What About Safety? Are Generics Really the Same?
Yes. The FDA tests every generic before it hits the market. They check the ingredients, the manufacturing process, the shelf life, and how the drug behaves in the body. If a generic doesn’t meet the exact same standards as the brand, it doesn’t get approved. Some people worry about small differences in inactive ingredients-like fillers or dyes. These don’t affect how the drug works. In rare cases, for drugs with a narrow therapeutic index-where the difference between a safe dose and a dangerous one is tiny-some patients report feeling different when switching between generic brands. But FDA data shows these cases are less than 1% of all generic prescriptions. If you notice a change, talk to your doctor. But don’t assume it’s the generic’s fault. Often, it’s just your body adjusting.How to Make Sure You’re Getting the Best Deal
1. Ask your pharmacist if a generic is available. They’re trained to know which ones are approved and interchangeable. 2. Check the FDA’s Orange Book-it lists all approved generics and their equivalence ratings. You don’t need to be a doctor to use it. 3. Compare prices. Not all generics cost the same. One brand might be $5, another $12. Ask for the lowest-cost option. 4. Use mail-order or discount programs. Many pharmacies offer $4 generic lists for common medications like metformin, lisinopril, or atorvastatin. 5. Don’t assume brand = better. If your doctor prescribes a brand, ask why. Is it because it’s necessary-or because they’re used to prescribing it?The Bigger Picture
Generic drugs aren’t just a cost-cutting trick. They’re a public health win. They make chronic disease management possible for people who can’t afford $500 pills. They reduce emergency room visits because patients can actually fill their prescriptions. They keep Medicare from collapsing under the weight of drug prices. The Congressional Budget Office projects that without generics, drug spending would grow at 6.8% per year. With them, it’s capped at 3.2%. That’s not a small difference. That’s the difference between a system that’s broken and one that’s sustainable. And yet, the conversation around drug prices still focuses on brand-name cost controls, not on expanding generic access. The truth? We already have the solution. It’s sitting on the pharmacy shelf, labeled in small print. All we need to do is choose it.Are generic drugs as safe as brand-name drugs?
Yes. The FDA requires generics to have the same active ingredients, strength, dosage form, and bioequivalence as the brand-name version. They must pass the same strict manufacturing and quality standards. Less than 1% of patients report any noticeable difference in effectiveness, and those cases are rare and often unrelated to the drug’s active ingredient.
Why do some generics cost more than others?
Price differences come from competition, manufacturing scale, and pharmacy contracts. Some generic manufacturers produce in bulk and sell at lower margins. Others may have fewer competitors in the market, allowing them to charge more. Always ask your pharmacist for the lowest-cost generic option-it’s often the same drug, just from a different company.
Can I switch from a brand-name drug to a generic without my doctor’s approval?
In most cases, yes. Pharmacists are legally allowed to substitute a generic for a brand-name drug unless the prescription says “dispense as written” or “no substitution.” But it’s still a good idea to inform your doctor, especially if you’re on a medication with a narrow therapeutic index, like warfarin or levothyroxine.
What’s the difference between a generic and a biosimilar?
Generics are exact copies of small-molecule drugs, like pills for blood pressure or diabetes. Biosimilars are highly similar versions of complex biologic drugs, like injectables for cancer or autoimmune diseases. They’re not identical because they’re made from living cells, but they work the same way and are approved by the FDA based on rigorous testing.
Why aren’t all drugs available as generics?
Brand-name drugs are protected by patents, which last 20 years from the date of filing. Some companies extend this protection through legal tactics like patent thickets or product hopping. Once those patents expire, generics can enter the market. But until then, only the original manufacturer can sell the drug.


9 Comments
Michael Gardner
Generics are a scam. I switched to a generic blood pressure med and my heart started acting up. Turns out the filler was corn-based and I’m allergic. They don’t test for that stuff properly.
Jennifer Taylor
YOU THINK THIS IS ABOUT HEALTH? 🤡 Big Pharma and the FDA are in bed together. They let generics in just enough to look good but keep the real profits in brand names. They’re manipulating you into thinking you’re saving money while they just shift the scam. I’ve seen the documents. They know generics cause more side effects. They just don’t tell you.
Jade Hovet
OMG YES!!! 💊 I’ve been on generic metformin for 3 years and my A1C is better than ever! 🙌 My pharmacist even gave me a $4 coupon-like, free meds?? 😭 Don’t let anyone tell you otherwise, generics saved my life. #GenericWins
Richard Ayres
The data presented here is compelling and aligns with peer-reviewed studies from the NEJM and JAMA. The Hatch-Waxman Act remains one of the most successful public health interventions in modern American history. The 90/12 paradox is not a market anomaly-it’s a structural correction to prior inefficiencies. It’s worth noting that the savings extend beyond direct costs: reduced hospitalizations, improved adherence, and lower long-term complications contribute significantly to systemic savings.
That said, the narrative around generics sometimes overlooks the challenges in manufacturing consistency across hundreds of suppliers. While the FDA’s bioequivalence standards are robust, real-world variability in dissolution rates can occasionally affect patient outcomes, particularly in narrow therapeutic index drugs. This doesn’t invalidate generics-it simply calls for better pharmacovigilance and patient education.
Shelby Ume
As someone who works in a community clinic, I see this every day. A patient comes in with a $150 co-pay for a brand-name statin. I ask if they’ve tried the generic. They look at me like I just offered them a magic wand. $8. They get it. They cry. They say, ‘I didn’t know I could afford this.’ That’s not just savings-that’s dignity restored. We need to train every provider to say ‘generic’ before they say ‘brand.’
And yes, I’ve had patients who swear the generic made them feel ‘off.’ Usually, it’s anxiety. Sometimes, it’s a different dye. But 99% of the time, they’re doing better within two weeks. We don’t talk about that enough.
Tyrone Marshall
Let’s not pretend this is just about pills. Generics are a mirror of our values. We live in a system where marketing trumps medicine, where profit is measured in patient suffering. The fact that $3.4 trillion was saved by people taking cheap pills? That’s not a win for capitalism. That’s a win for humanity.
And yet, we still let drug companies write the rules. Patent thickets? Product hopping? These aren’t loopholes-they’re crimes disguised as business. The real question isn’t why generics work. It’s why we let monopolies exist at all in healthcare.
Every time you choose a generic, you’re voting against greed. You’re saying: my life is worth more than their quarterly earnings. That’s not just smart. It’s revolutionary.
nina nakamura
Generics are dangerous. The FDA doesn’t test them the same way. The bioequivalence window is too wide. I’ve seen patients crash after switching. They blame the patient. They say it’s ‘psychological.’ No. It’s negligence. The system is designed to save money, not lives. And you’re all just happy because you got a $2 pill. Wake up.
Willie Onst
Man, I used to think generics were just for broke people. Then my grandma got on one for her diabetes and started walking again. She said, ‘I didn’t know I could feel like this.’ Now I get all my meds generic-even my anxiety pills. I used to feel guilty. Now I feel like a hero. We’ve been lied to about what ‘quality’ means. It’s not about the label. It’s about what works. And generics? They work.
And hey-if you’re still paying full price because you think brand = better, you’re not being loyal to your health. You’re being loyal to an ad.
Himmat Singh
While the statistical claims are impressive, they fail to account for the long-term degradation of pharmaceutical innovation. The incentive structure created by generic competition has led to a stagnation in R&D investment among domestic manufacturers. The $3.4 trillion in savings is offset by a decline in novel drug development, particularly in areas like neurodegenerative diseases and rare pediatric conditions. The trade-off is not as benign as presented.