When you’re prescribed a life-saving medication and there’s no generic version available, the cost can feel impossible. Some drugs cost more than $10,000 a month. For many, that’s not just a bill-it’s a choice between medicine and rent. But there’s help. Patient Assistance Programs (PAPs) exist specifically for situations like this. They’re not a secret. They’re not a last resort. They’re a structured, legal, and widely used system designed to get you the medication you need when you can’t afford it.
Why PAPs Matter When There’s No Generic
Generic drugs bring down prices by 80-90%. But when a drug has no generic-like Soliris for rare blood disorders, or Tasigna for leukemia-the price stays sky-high. These are often specialty drugs developed for small patient groups. Pharmaceutical companies set the list price, and without competition, it doesn’t drop. That’s where PAPs step in. In 2022, these programs gave out $4.7 billion in aid, mostly for brand-name drugs with no generic alternatives. For uninsured patients, PAPs are often the only way to get the medicine at all.How PAPs Actually Work
PAPs aren’t one-size-fits-all. There are three main types:- Manufacturer-sponsored (65% of programs): Run directly by drug companies like Novartis, Gilead, or Eli Lilly. These usually cover 100% of the drug cost if you qualify.
- Foundation-sponsored (25%): Run by nonprofits like the Patient Access Network Foundation or the Chronic Disease Fund. These often help people with insurance but high out-of-pocket costs.
- State-sponsored (10%): Programs like PACE in Pennsylvania help seniors with limited income.
- Have an income below 400% of the Federal Poverty Level (about $60,000 for one person in 2023)
- Be uninsured or underinsured
- Have a valid prescription
- Get your doctor to sign paperwork
The Big Catch: Accumulator Adjustments
Here’s where things get messy. If you have commercial insurance, your drug costs should count toward your deductible and out-of-pocket maximum. But most major pharmacy benefit managers (PBMs)-like Express Scripts and Optum-now use accumulator adjustment policies. That means the money a PAP pays for your drug doesn’t count toward your annual limits. Example: Your drug costs $12,000 a month. Your PAP covers it. Your insurance says you’re not paying anything. Sounds good, right? But your deductible is still $8,700. You haven’t made progress. Next year, you’ll start over. You might pay $20,000 out-of-pocket before your insurance even kicks in. This trick has left thousands of patients trapped.Who Can’t Use Manufacturer PAPs?
Medicare beneficiaries are blocked from using manufacturer copay assistance for Part D drugs. That rule took effect in 2020 and was reinforced in 2025 under the Inflation Reduction Act. If you’re on Medicare, you can’t get help from the drugmaker. But you can still apply to foundation-sponsored PAPs. These don’t follow the same rules. Programs like the Patient Access Network Foundation or the HealthWell Foundation can help Medicare patients with brand-name drugs.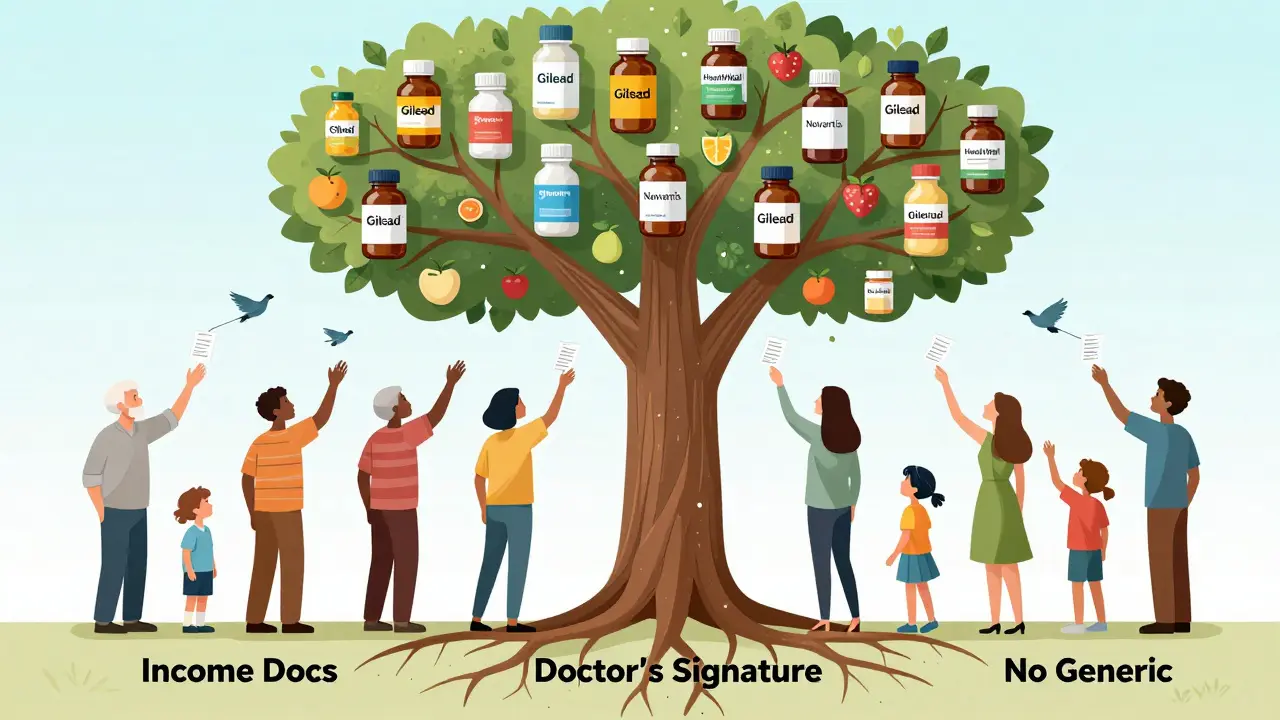
How to Find and Apply for a PAP
Start with a free tool like RxHope or NeedyMeds. These sites let you search by drug name and show you which PAPs cover it. You’ll see eligibility rules, required documents, and contact info. Once you find a match:- Download the application form from the program’s official website.
- Call your doctor’s office. Ask if they have a medication access specialist. Most hospitals now do. They can help fill out the paperwork-saving you hours.
- Gather your documents: tax return, pay stubs, prescription, insurance card (or denial letter if uninsured).
- Submit the application. Manufacturer PAPs usually approve within 7-10 days. Foundation programs take 2-3 weeks.
- Follow up. If you don’t hear back in 10 days, call. Many applications get lost or incomplete.
What to Do If You’re Insured
If you have insurance, you might think PAPs aren’t for you. But if your plan has high deductibles or copays, they still can be. The key is finding a foundation PAP that works with your insurance. These programs pay your copay directly, so you don’t have to pay upfront. But watch out for accumulator adjustments. Ask your insurer: “Do you have an accumulator policy?” If yes, ask if they’ll waive it for your specific drug. Sometimes they will-if you push.Alternative Options When PAPs Don’t Fit
If you don’t qualify for a PAP, or the process feels overwhelming:- Pharmacy discount cards (like GoodRx): These give small discounts-around 8% on brand-name drugs with no generic. Not enough for $15,000/month drugs, but better than nothing.
- State pharmaceutical programs: These often have lower income limits than PAPs. For example, PACE in Pennsylvania helps seniors earning under $28,500/year.
- Nonprofit grants: Organizations like the Cancer Financial Assistance Coalition or the Leukemia & Lymphoma Society offer one-time grants for specific conditions.

Real Stories: What Works
One patient with HIV was paying $15,000 a month for his medication. He had no insurance. Through Gilead’s Advancing Access program, he got the drug for $0. He kept his apartment. He stayed on treatment. Another patient with chronic myeloid leukemia was paying $1,400 a month for Tasigna. She couldn’t afford it. After 11 hours of paperwork over three weeks, she got into Novartis’s PAP. Her cost dropped to $0. But she had to call the pharmacy twice a week to make sure the drug shipped on time. A Medicare patient with cancer tried to use a manufacturer copay card. It was denied. She switched to a foundation PAP. She’s now paying $50 a month instead of $12,000.What’s Changing in 2026
Drug companies are making PAPs easier. Eli Lilly’s “Simple Bridge” program cuts a 17-step application down to five steps. Approval time? Under 48 hours. Epic Systems, the biggest electronic health record company, is now building PAP tools directly into doctors’ software. That means your doctor can check your eligibility and submit the application while you’re still in the exam room. But the system is still broken. Drug prices keep rising. PAPs are a band-aid. They help millions-but they don’t fix the root problem: drugmakers set prices with no accountability.Final Tips
- Don’t wait until you run out of pills to start. Apply early. Processing takes time.
- Keep copies of everything. Save emails, letters, receipts.
- Ask your pharmacist. They know which PAPs are easiest to get into.
- If your doctor says, “We don’t help with that,” find another provider. Many hospitals now have dedicated patient navigators.
- Use multiple resources. Apply to more than one PAP. If one denies you, another might approve.
Frequently Asked Questions
Can I use a patient assistance program if I have insurance?
Yes, but only if your insurance doesn’t cover the drug fully or you have high out-of-pocket costs. Manufacturer PAPs usually require you to be uninsured. Foundation PAPs can help even if you have insurance, especially if your plan has an accumulator adjustment policy that blocks PAP payments from counting toward your deductible.
Do I have to reapply every year?
Yes. Most PAPs require annual recertification. You’ll need to submit updated income documents and a new prescription. Some programs send reminders, but don’t rely on them. Mark your calendar to reapply three months before your current approval expires.
What if I make too much money for a PAP?
If you’re over the income limit, you might still qualify for a foundation PAP or a state program. Some foundations use sliding scales and can help patients earning up to 500% of the Federal Poverty Level. Also, ask your doctor about patient assistance grants from drugmakers-they sometimes have discretionary funds for those who just miss eligibility.
Can Medicare patients get help?
Medicare patients cannot use manufacturer copay assistance for Part D drugs. But foundation-sponsored PAPs like the Patient Access Network Foundation and HealthWell Foundation can help. These programs don’t violate Medicare rules and often cover high-cost brand-name drugs with no generic alternatives.
How long does it take to get approved?
Manufacturer PAPs usually approve within 7-10 business days. Foundation programs take longer-14-21 days-because they review more documents. If you’re in urgent need, call the program directly and ask about expedited processing. Many have emergency pathways for patients at risk of stopping treatment.


13 Comments
Sean Feng
Just got approved for a PAP after 3 weeks of calling everyone. My drug costs $11k/month. Now I pay $0. No drama. Just do the paperwork.
Priya Patel
This made me cry. I’m in India and my cousin in the US is on a $14k/month drug. She’s been applying for months. I just shared this with her. Thank you for writing this like someone who’s been there. 💪
Priscilla Kraft
PLEASE NOTE: If you're on Medicare, don't give up. Foundation PAPs like HealthWell and PAN are your lifeline. I helped my mom get Tasigna for $30/month after being denied by the manufacturer. It took 11 calls, 3 emails, and one very angry conversation with a PBM rep-but we got it. You can too. 🙌
Michael Patterson
Look, I get it, PAPs are great, but let's be real here-this whole system is a scam. Pharma companies make billions, then pretend to be saints by giving out free meds to people who are barely above poverty. Meanwhile, they jack up prices every year and lobby Congress to keep the rules this way. This isn't help-it's PR. And the accumulator thing? That's not a bug, it's a feature designed to bankrupt you slowly. Wake up.
Matthew Miller
So you’re telling me a 65-year-old with $58k income and insurance can’t get help unless they’re broke and uninsured? And if they’re on Medicare, they’re screwed? And the only way out is to beg a nonprofit? This isn’t healthcare. This is a horror show written by a committee of CEOs who think ‘affordable’ means ‘pay $2000/month.’
Adewumi Gbotemi
I am from Nigeria. We don’t have this kind of system. If you need medicine and can’t pay, you don’t get it. I read this and I am shocked. America has so much but still people suffer. This is sad. I hope your system gets better.
Roshan Joy
One thing people forget: your pharmacist is your secret weapon. I didn’t know this until I asked mine. She pulled up a list of 3 PAPs for my drug I didn’t even know existed. One approved me in 48 hours. Don’t just go to RxHope-talk to the person behind the counter. They know the shortcuts.
Christian Basel
Accumulator adjustment policies are a form of financial predation disguised as cost containment. PBMs are essentially extracting value from patient assistance mechanisms by rendering them fungible to deductible progress, thereby creating a perverse incentive structure where the insurer internalizes the benefit of the PAP payment while externalizing the financial burden onto the patient. This is not merely inequitable-it’s a structural violation of the fiduciary duty owed to beneficiaries.
Alex Smith
So let me get this straight. You’re telling me that if I make $61k, I’m too rich for help, but if I make $59k, I get my $12k/month drug for free? And if I’m on Medicare, I’m basically a second-class citizen? Wow. The American healthcare system is like a video game where the final boss is a spreadsheet.
Madhav Malhotra
My uncle in India is on a similar drug. He pays $800/month out of pocket. We all chip in. It’s not ideal, but we make it work. I wish there was something like this in India. Maybe someday. Thanks for sharing this-it’s a roadmap for people who feel lost.
Jennifer Littler
Just want to add: if your doctor says they don’t help with PAPs, find a new doctor. Seriously. I had one who told me to ‘just go on disability.’ I switched to a hospital-based clinic with a medication access navigator. They filed my paperwork in 20 minutes. It’s not about your meds-it’s about who you’re working with.
Jason Shriner
the system is broken but i still have to pay my rent so i guess i’ll just… keep breathing? lol
Alfred Schmidt
WHY IS THIS NOT PUBLIC KNOWLEDGE?!?!?!?!!? I’ve been paying $9,000 a month for 18 months and I just found out I could’ve gotten this for FREE?!?!?!? I wasted my life! I lost my job! My partner left me! I could’ve been in a cabin in the woods with my cat and my meds and my dignity! WHY DID NO ONE TELL ME?!?!?!!?!?!!