Diuretic Hydration Calculator
This calculator helps you determine the right amount of fluid to drink based on your diuretic type, activity level, and health status. Follow the recommendations to avoid dehydration or fluid overload.
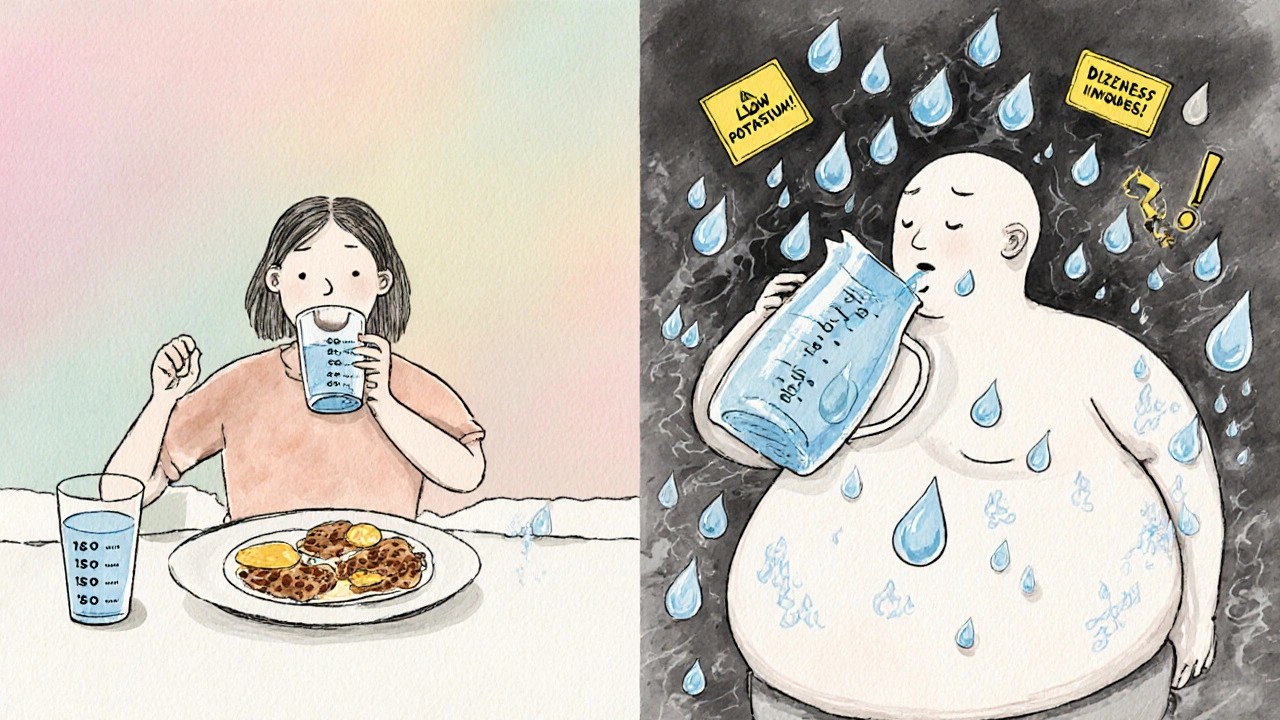
When you’re on diuretics - often called "water pills" - your body is working overtime to get rid of extra fluid. That’s the whole point. But here’s the catch: if you don’t replace what you’re losing, you can end up dehydrated, dizzy, or even in the hospital. It’s not about drinking more water than usual. It’s about drinking the right amount, at the right time, with the right balance of electrolytes.
What Diuretics Do to Your Body
Diuretics like furosemide, hydrochlorothiazide, and spironolactone don’t just make you pee more. They change how your kidneys handle sodium and water. Loop diuretics like furosemide block sodium reabsorption in the thick part of the kidney tubule, forcing out up to 2 liters of extra urine a day. Thiazides, like hydrochlorothiazide, work lower down and remove about 50-100 mEq of sodium daily. Potassium-sparing diuretics like spironolactone stop your body from losing too much potassium, but they can cause the opposite problem: too much potassium.
That’s why one size doesn’t fit all. Someone on furosemide for heart failure might lose 1.5 liters of fluid in a single day. Someone on a low-dose thiazide for high blood pressure might only lose 300-500 mL. The bigger the diuretic effect, the more attention you need to pay to what you’re drinking - and what you’re not.
The Hydration Trap: Too Little or Too Much
Most people assume the answer is simple: drink more water. But that’s where things go wrong. In a 2023 patient survey by the American Heart Association, 62% of diuretic users reported dizziness, 45% had muscle cramps, and 38% got headaches - all signs of low fluid volume. But here’s the twist: 18% of heart failure readmissions happen because patients drank too much water trying to feel better.
It’s a tightrope walk. Too little fluid? You get dehydrated. Your blood pressure can actually rise because your heart has to work harder to pump thicker, lower-volume blood. Too much fluid? Your heart and kidneys get overloaded again. You swell up. Your blood pressure spikes. You’re back where you started.
One Reddit user, CardioWarrior87, described it perfectly: "Constant thirst but terrified to drink too much - ended up in the ER with low potassium after drinking 3 liters in one day while on furosemide." That’s not an isolated story. It’s the norm for people trying to self-manage without clear guidance.
How Much Should You Actually Drink?
There’s no universal number. But most experts agree on a starting point: 1.5 to 2 liters (6-8 cups) per day for healthy adults on diuretics. That’s about the same as what you’d drink without medication - but timing matters more than volume.
Drinking 1.5 liters all at breakfast? Bad idea. Your kidneys will flush it out fast, leaving you dry by afternoon. Spreading it out - 200-300 mL every 2-3 hours - keeps your body steady. Morning is the safest window. Avoid large drinks after 6 p.m. to prevent nighttime trips to the bathroom that disrupt sleep and raise fall risk.
But if you have kidney disease (eGFR below 30 mL/min/1.73m²), your doctor may limit you to 1-1.5 liters a day. If you’re on a strong loop diuretic, you might need to add 300-500 mL extra to replace losses. Always check with your provider - your numbers are unique.
Electrolytes Are Just as Important as Water
Water alone won’t fix what diuretics break. You’re losing sodium, potassium, magnesium, and chloride every time you pee. Thiazides can drop potassium levels by 20-40 mEq per day. Loop diuretics? Up to 100 mEq. That’s why muscle cramps, irregular heartbeat, and fatigue are so common.
Potassium-sparing diuretics like spironolactone help - but they can push potassium too high, especially if you have kidney trouble or eat a lot of bananas, spinach, or salt substitutes. The key isn’t to avoid potassium. It’s to balance it.
Many patients now use oral rehydration solutions like DripDrop ORS, which contain 1,000 mg sodium, 200 mg potassium, and 250 mg glucose per liter. These aren’t sports drinks. They’re medical-grade replacements designed to mimic what your body loses. You don’t need them every day, but having them on hand for hot days, illness, or heavy sweating can prevent a trip to the ER.
What to Avoid - Alcohol, Caffeine, and More
Alcohol and caffeine are diuretics too. A single beer or two cups of strong coffee won’t hurt. But if you’re already on a prescription diuretic, adding alcohol can increase dehydration by 40-60%, according to Silver Ridge Recovery’s 2024 report. That’s why 34% of diuretic users end up in emergency rooms after combining the two.
Caffeine over 250 mg a day (about 2-3 strong coffees) adds up. It doesn’t cancel out your diuretic, but it makes fluid loss harder to predict. If you drink coffee, make sure you’re replacing it with water. And never use alcohol as a way to "help" with swelling. It makes everything worse.
How to Know If You’re Getting It Right
You don’t need fancy tools - just two simple habits.
1. Weigh yourself every morning. Do it before breakfast, after using the bathroom, in the same clothes (or none). A sudden drop of more than 1 kg (2.2 lbs) overnight means you’re losing too much fluid. A gain of 1 kg or more means you’re holding on to too much. Both need attention.
2. Check your pee color. Clear or pale yellow? You’re hydrated. Dark yellow or amber? You need more fluid. Use this as your daily guide. Don’t wait for thirst - by then, you’re already behind.
Some patients use smart cups like the HydraSmart Cup (FDA-approved in January 2024), which tracks fluid intake and syncs with their health records. These reduce dehydration-related ER visits by 35%. But even a simple notebook and pen work. Write down your weight, fluid intake, and pee color each day. After a few weeks, patterns emerge. You start to know your body’s rhythm.

When to Call Your Doctor
Don’t wait for a crisis. Call your doctor if you notice:
- Weight loss of more than 1 kg (2.2 lbs) in 24 hours
- Heart palpitations, dizziness, or fainting
- Severe muscle cramps or weakness
- Confusion, headache, or nausea
- Urine output drops below 300 mL/day
These aren’t "just side effects." They’re signs your fluid-electrolyte balance is off. Your doctor might adjust your dose, add a supplement, or change your medication. But they can’t help if you don’t speak up.
What’s New in Hydration Management
Technology is catching up. AI-driven apps now analyze your weight, urine output, and blood tests to give real-time fluid recommendations. In a 2024 trial of 300 patients, those using AI tools had 42% fewer electrolyte imbalances.
Pharmaceutical companies are testing combination pills - like PotassiSure, which pairs spironolactone with timed potassium release. Early results show 58% fewer cases of low potassium compared to regular spironolactone. These aren’t available yet, but they’re coming.
Meanwhile, 68% of primary care doctors now give structured hydration advice when prescribing diuretics - up from 42% in 2020. That’s progress. But the burden still falls on you to track, adjust, and communicate.
Real Success Stories
One patient, "DiureticDiva," posted on PatientsLikeMe in March 2024: "I used to go to the hospital 4 times a year for dehydration and low potassium. I started weighing myself every morning, tracking my pee color, and carrying an electrolyte drink. Now, 18 months later - zero ER visits. It’s not magic. It’s routine."
She didn’t stop her meds. She didn’t drink more water. She learned how to match her intake to her output. That’s the secret.
Can I drink coffee while on diuretics?
Yes, but limit it to 1-2 cups a day (under 250 mg caffeine). Coffee acts as a mild diuretic, so if you drink it, replace each cup with a glass of water. Avoid large amounts, especially if you’re already losing a lot of fluid from your medication.
Should I take potassium supplements with my diuretic?
Only if your doctor tells you to. Some diuretics cause potassium loss, others cause too much. Taking extra potassium without testing can be dangerous - it can trigger heart rhythm problems. Always get a blood test before starting supplements.
How long does it take to get used to fluid balance on diuretics?
Most people need 4-6 weeks to find their rhythm. The first week is the hardest - you’ll feel thirsty, tired, or even dizzy. That’s normal. Stick to your fluid schedule, track your weight, and avoid big drinks. After a month, your body adjusts, and symptoms improve.
Is it safe to drink alcohol with diuretics?
No. Alcohol increases fluid loss and can cause severe dehydration, especially with loop diuretics like furosemide. Studies show people who drink alcohol while on diuretics are 2.7 times more likely to end up in the ER. Even one drink can throw off your balance. Skip it.
What should I do if I’m sweating a lot or feel sick?
Increase your fluid intake by 300-500 mL for every 500 mL of extra fluid lost (from sweat, fever, or vomiting). Use an electrolyte solution if you can. Weigh yourself before and after. If your weight drops more than 1 kg or you feel faint, call your doctor. Don’t wait.
Do I need to change my diet if I’m on diuretics?
Yes - but not always in the way you think. Avoid very salty foods - they make your body hold water, which defeats the purpose. But don’t go low-sodium unless your doctor says so. You’re losing sodium with your urine. Focus on balance: eat vegetables, lean proteins, and whole grains. Avoid salt substitutes if you’re on potassium-sparing diuretics.
Managing hydration on diuretics isn’t about perfection. It’s about awareness. You’re not just taking a pill - you’re managing a delicate system. Track your weight. Watch your pee. Spread out your fluids. Avoid alcohol. Talk to your doctor. Small habits, done consistently, prevent big problems. Millions of people do it every day. You can too.


12 Comments
Ravi boy
bro i just drink when i thirsty n if i pee a lot i chill for a bit its not that hard
Matthew Karrs
they say drink 1.5-2L but did you know the FDA secretly allows pharma companies to push fluid guidelines to sell more electrolyte drinks? i checked the 2024 trial funding... it's all tied to DripDrop's parent company. wake up.
Matthew Peters
i was on furosemide for 8 months and thought i was doing great until i collapsed at the gym. turned out i was drinking 3L a day thinking i was "hydrated". my doc laughed and said "you're not a camel, you're a human with a broken kidney." now i weigh myself every morning. no more drama. just numbers.
Liam Strachan
i've been on spironolactone for hypertension and honestly? the pee color trick changed everything. used to stress over exact ml, now i just look at the toilet. pale yellow = good. tea color = drink. dark amber = call the doc. simple. no apps needed.
Gerald Cheruiyot
fluid balance isnt about rules its about listening your body isnt a machine its a conversation you show up with awareness and it shows up with signals you dont need an app to know when your lips are dry
Michael Fessler
for those on loop diuretics, you're losing 60-100 mEq Na+ daily. that's why oral rehydration solutions with 1000mg Na+ and 200mg K+ are clinically superior to Gatorade. Gatorade has 270mg Na+ and 70mg K+ per liter - it's a sugar bomb with a side of electrolytes. DripDrop? it's designed for renal patients. if you're not using it on high-dose furosemide, you're playing russian roulette with your serum sodium.
daniel lopez
EVERYONE knows the real problem is the government and big pharma forcing people to drink water so they can sell more electrolyte packs. my cousin's cardiologist told him to drink less and eat salt. he's been fine for 5 years. they don't want you to know this.
Nosipho Mbambo
I've been on HCTZ for 12 years. I drink exactly 1.8L per day. I track it. I weigh myself. I avoid bananas. I don't drink coffee after 2 PM. I don't drink alcohol. I don't use salt substitutes. And I still get cramps. So... what's the point of all this "science" if it doesn't actually fix anything?
Russ Bergeman
i read this whole thing and still have no idea how much to drink. my doctor just says "drink when you're thirsty." why is this so complicated?
Dana Oralkhan
i want to say thank you to whoever wrote this. my mom was in the hospital twice last year from dehydration on her diuretics. we started doing the weight check and pee color thing last month. she hasn't been back to the ER. it's not glamorous. it's not new. but it saved her. thank you for making it simple.
Jeremy Samuel
nah man you dont need all this. just drink beer. it's a diuretic too so it balances out. plus you get to chill. win win.
Destiny Annamaria
this is the most helpful thing i've read in years. i'm 68, on furosemide, and i used to think "more water = better". now i know it's about rhythm. i spread my sips like i'm sipping tea in the morning. no more midnight bathroom runs. i feel like a new person.