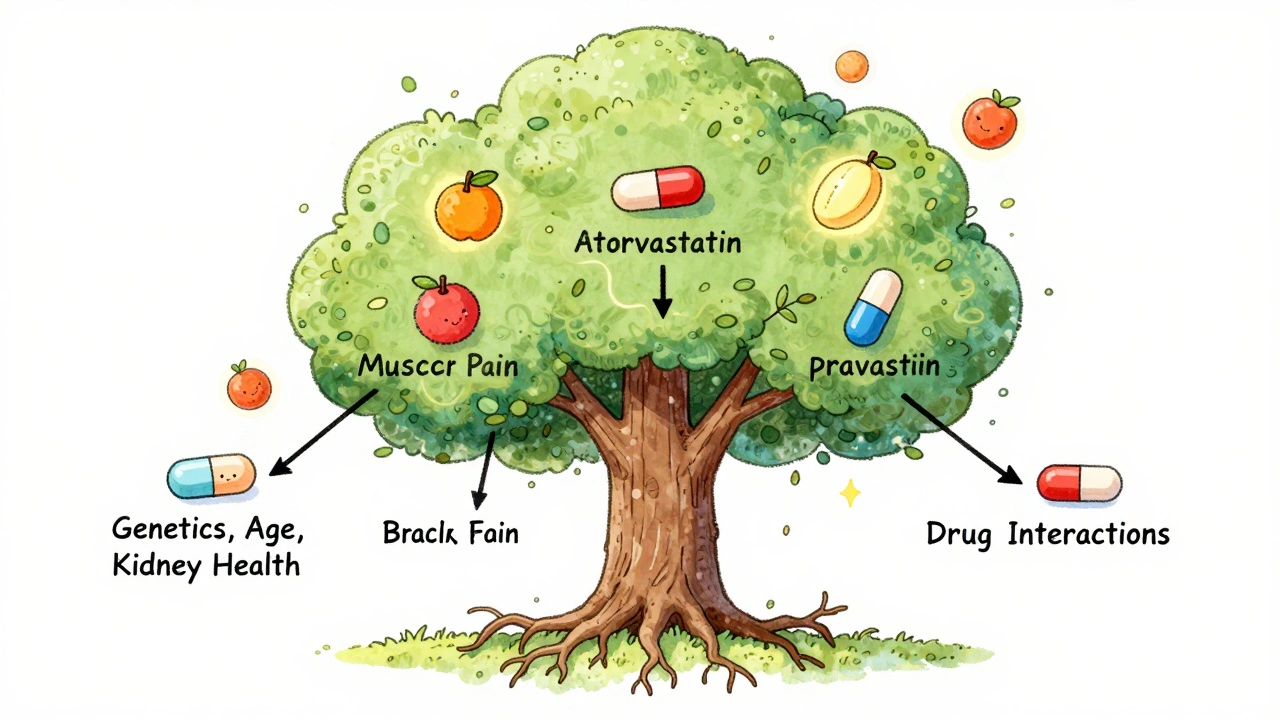
When you’re prescribed a statin, you’re not just getting a cholesterol-lowering pill-you’re getting a drug with a hidden personality. Some statins are like quiet guests who stick to the kitchen (the liver), while others wander into every room of the house, including your muscles and nerves. This isn’t just chemistry-it’s the difference between feeling fine and waking up with sore legs you can’t explain.
What Makes a Statin Hydrophilic or Lipophilic?
It all comes down to solubility. Lipophilic statins dissolve in fat. That means they slip easily through cell membranes, not just in the liver, but everywhere else too-muscles, brain, kidneys. Hydrophilic statins, on the other hand, prefer water. They can’t just float through cell walls. They need special doors-called OATP transporters-to get into liver cells. That’s why they mostly stay put in the liver, where you want them to work.
Here’s the short list:
- Lipophilic statins: simvastatin, atorvastatin, fluvastatin, lovastatin, pitavastatin
- Hydrophilic statins: pravastatin, rosuvastatin
That’s it. Only two hydrophilic options. The rest? All fat-loving. And that small difference in solubility changes how your body reacts.
Why Muscle Pain Happens-And Why It’s Not Always What You Think
For years, doctors told patients: "If you get muscle pain, it’s probably because you’re on a lipophilic statin." The logic was simple: fat-soluble drugs get into muscle tissue more easily, so they cause more damage. It made sense. But real-world data doesn’t always follow logic.
Studies show mixed results. One big study of 15 million patients found that pravastatin (hydrophilic) had a lower risk of muscle problems than simvastatin (lipophilic). But then, rosuvastatin (also hydrophilic) had a higher risk than atorvastatin (lipophilic). That’s not a typo. Hydrophilic doesn’t automatically mean safer.
Here’s what’s really going on: it’s not just about whether a statin is fat-soluble. It’s about dose, age, genetics, and other meds you’re taking. A 72-year-old woman on amiodarone for heart rhythm issues? She’s at higher risk for muscle pain no matter which statin she takes. Same with someone who’s thin, has kidney issues, or is on multiple drugs that compete for the same liver enzymes.
And here’s the kicker: many people who blame their statin for muscle pain don’t actually have a true statin-related myopathy. Their CK levels are normal. Their symptoms are mild. Sometimes, it’s just aging, vitamin D deficiency, or overtraining at the gym. But because statins are blamed so often, switching becomes the default answer-even when it’s not needed.
What the Data Really Says About Side Effects
Let’s cut through the noise. What do the numbers actually show?
| Side Effect | Hydrophilic (Pravastatin, Rosuvastatin) | Lipophilic (Simvastatin, Atorvastatin) |
|---|---|---|
| Muscle pain (myalgia) | Variable-rosuvastatin can be as high as atorvastatin | Higher in simvastatin; similar to rosuvastatin in some studies |
| Drug interactions | Lower (especially pravastatin-minimal CYP3A4 use) | Higher (simvastatin and atorvastatin heavily rely on CYP3A4) |
| Cognitive effects (brain fog) | Potentially lower due to less brain penetration | Potentially higher-crosses blood-brain barrier more easily |
| Renal safety | Preferred in kidney disease-better outcomes | Less preferred in eGFR <60 |
| LDL reduction (at standard dose) | Rosuvastatin: 52% at 20mg; Pravastatin: 34% at 20mg | Atorvastatin: 47% at 20mg; Simvastatin: 41% at 20mg |
The takeaway? Rosuvastatin, despite being hydrophilic, is one of the most potent statins-and it’s also one of the most commonly reported for muscle pain. Simvastatin, the classic lipophilic statin, has the highest risk of interactions and side effects, especially at doses above 20mg. But atorvastatin? It’s a middle ground. High potency, moderate interactions, and mixed muscle risk.
Real People, Real Stories
Online forums are full of contradictions. One person swears switching from simvastatin to pravastatin solved their muscle pain. Another says rosuvastatin wrecked their legs-even though it’s hydrophilic. And then there’s Dave, who posted on his blog: "I had worse pain on rosuvastatin than I ever did on simvastatin. I switched to pravastatin and it finally stopped."
That’s the problem with generalizations. One person’s solution is another’s nightmare. A 2023 Reddit thread with 142 responses showed 78% of people on lipophilic statins reported muscle pain, compared to 42% on hydrophilic. But that’s self-reported. People who have bad reactions are more likely to post. Those who feel fine? They don’t say anything.
Still, the pattern holds: if you’re prone to side effects, pravastatin often feels gentler. Rosuvastatin? It’s powerful, but it’s not gentle. And if you’ve had trouble with one statin, don’t assume switching to another type will fix it. Sometimes, you just need a lower dose-or a different approach entirely.
Who Should Switch? Who Shouldn’t?
You don’t need to switch statins just because of lipophilicity. But here are times when it makes sense:
- You’re over 65, thin, or on multiple medications (like amiodarone or fibrates).
- You have kidney disease-hydrophilic statins (especially pravastatin) are safer here.
- You’re on a high dose of simvastatin (over 20mg)-that’s the biggest offender for muscle issues.
- You’re experiencing brain fog or sleep issues-lipophilic statins may be crossing into your brain.
- You’ve had muscle pain with one statin and want to try a gentler option.
Don’t switch if:
- You’re doing great on your current statin-no side effects, LDL is under control.
- You’re on low-dose atorvastatin and feel fine. No need to fix what isn’t broken.
- You’re on rosuvastatin for very high cholesterol and it’s working. The benefits outweigh the risks.
Switching statins isn’t about following a rule. It’s about listening to your body and matching the drug to your profile.
What to Do If You Have Muscle Pain
If you’re having muscle soreness, don’t panic. First, rule out other causes: dehydration, overexertion, thyroid issues, vitamin D deficiency. Then, check your creatine kinase (CK) levels. If they’re normal and your pain is mild, you probably don’t have true statin myopathy.
Here’s what works:
- Lower the dose. Sometimes, half a tablet is enough.
- Try every-other-day dosing. Many people tolerate this just fine.
- Take CoQ10 (200mg daily). It’s not magic, but it helps some people.
- Switch to pravastatin. It’s the gentlest statin with the lowest interaction risk.
- If nothing works, talk to your doctor about non-statin options like ezetimibe or bempedoic acid.
Studies show 68% of people who switch or adjust their dose get relief. That’s a good sign. But don’t give up on statins entirely. They prevent heart attacks and strokes. The goal isn’t to avoid them-it’s to find the right one for you.
The Future: Beyond Lipophilicity
Doctors are starting to move past the lipophilic vs hydrophilic debate. New research is looking at genetics-like variations in the SLCO1B1 gene-that tell you if you’re more likely to get muscle pain from statins. That’s the real future: personalized medicine.
Right now, we’re still stuck with broad categories. But the data is clear: lipophilicity isn’t destiny. Rosuvastatin, the hydrophilic statin, is the second most prescribed in the U.S. Simvastatin, the classic lipophilic, is falling out of favor-not because it’s fat-soluble, but because it’s risky at higher doses.
What matters most is your individual risk, your goals, and how your body responds. If you’ve had side effects, you’re not alone. And you don’t have to live with them. There are options. You just need to know where to look.
Are hydrophilic statins always safer than lipophilic ones?
No. While hydrophilic statins like pravastatin are often gentler on muscles and have fewer drug interactions, rosuvastatin-a hydrophilic statin-can cause muscle pain just as often as lipophilic statins like atorvastatin. Safety depends on dose, age, kidney function, and genetics-not just solubility.
Which statin has the least side effects?
Pravastatin is generally considered the gentlest statin. It’s hydrophilic, has minimal liver enzyme interactions, and is less likely to cause muscle pain or cognitive side effects. But it’s also less potent than rosuvastatin or atorvastatin, so it’s not always the best choice for people with very high cholesterol.
Can I switch from atorvastatin to pravastatin on my own?
No. Never switch statins without talking to your doctor. Stopping or changing statins without supervision can raise your cholesterol and increase your risk of heart attack or stroke. Your doctor will check your LDL levels, kidney function, and other meds before making a change.
Why do some people get muscle pain with rosuvastatin if it’s hydrophilic?
Rosuvastatin is highly potent, and even though it’s hydrophilic, it still enters muscle cells in significant amounts-especially at higher doses. Its potency can overwhelm muscle cells, leading to damage regardless of solubility. Also, some people have genetic variants that make them more sensitive to statins, no matter the type.
Should I take CoQ10 with my statin?
It’s worth trying if you have muscle pain. Statins lower CoQ10 levels in the body, which may contribute to muscle fatigue and soreness. Taking 200mg daily of CoQ10 helps some people, though studies aren’t conclusive. It’s safe, inexpensive, and has no serious side effects-so many doctors recommend it as a first step.
Is there a statin that doesn’t cause muscle pain at all?
No statin is completely free of muscle pain risk. Even the gentlest ones, like pravastatin, can cause side effects in rare cases. But the risk is much lower with pravastatin, fluvastatin, or low-dose rosuvastatin. If you’ve had pain with one, another might work better. It’s trial and error-with your doctor’s guidance.
Final Thought: It’s Not the Type-It’s You
Statins are not one-size-fits-all. The idea that hydrophilic = safe and lipophilic = dangerous is outdated. The truth is messier. Your age, weight, kidney function, other medications, and even your genes matter more than whether a drug dissolves in fat or water.
If you’re on a statin and feel fine-keep taking it. If you’re having side effects, don’t assume it’s the type. Talk to your doctor. Try a lower dose. Consider pravastatin. Check your vitamin D. Try CoQ10. Sometimes, the fix is simple. Other times, you need a new plan. But you don’t have to live with pain. There’s always a way forward.


8 Comments
Karl Barrett
Let’s be real-the hydrophilic/lipophilic dichotomy is a useful heuristic, but it’s like saying ‘all cars are either gas or electric’ and ignoring that a Tesla can still break down if you ignore tire pressure. The SLCO1B1 polymorphism? That’s the real MVP here. I’ve seen patients on pravastatin with CK levels through the roof because they’re homozygous for *521T. Meanwhile, some folks on simvastatin 80mg feel fine as long as their CYP3A4 isn’t drowning in grapefruit juice. It’s pharmacogenomics, not solubility, that’s gonna dictate the future of statin prescribing.
Jake Deeds
Oh wow, someone finally said it out loud. Rosuvastatin is basically the Ferrari of statins-powerful, expensive, and if you’re not careful, it’ll leave your muscles in the ditch. And yet, every cardiologist I know treats it like it’s the holy grail. Meanwhile, pravastatin’s over there, quietly saving lives like a reliable Honda Civic nobody talks about. If you’re 70, on amiodarone, and your doctor pushes rosuvastatin? That’s not medicine. That’s arrogance with a stethoscope.
George Graham
I’ve been a nurse for 22 years, and I’ve seen this play out a hundred times. A patient comes in complaining of ‘statin legs’-they can barely climb stairs. We check CK, it’s normal. They’re taking ibuprofen daily, haven’t slept well in months, and their vitamin D is 18. We lower the dose, add CoQ10, and tell them to walk 15 minutes a day. Three weeks later? They’re back, thanking us. No switch needed. Sometimes the drug isn’t the problem-it’s the life around it. We treat the pill, not the person. That’s the real tragedy.
John Filby
CoQ10 200mg daily? I’ve been taking it since I switched from atorvastatin to pravastatin and honestly? My legs don’t feel like lead anymore 😊 I’m not saying it’s magic, but I’ve tried everything else-stretching, magnesium, even acupuncture-and this was the only thing that made a difference. Also, my doc said to take it at night, which I didn’t know. Who knew?
Elizabeth Crutchfield
i had the worst muscle pain on rosuvastatin… like, couldnt even open a jar kind of pain. switched to pravastatin and it was like a miracle. why do docs keep pushing the strong ones? just b/c they lower ldl faster doesnt mean theyre better for YOU. my doctor was like ‘but its the most effective!’ and i was like… but i cant walk to my mailbox. 🥲
Ben Choy
Man, this thread is gold. I was on simvastatin 40mg for 3 years, then switched to rosuvastatin 10mg after muscle pain. Thought I was safe because it’s ‘hydrophilic.’ Nope. Same issue. Ended up on low-dose fluvastatin-yes, that old-school one-and I feel better than ever. Point is: don’t trust labels. Trust your body. And if your doc doesn’t listen? Find a new one. You’re not a statistic. You’re a human.
Emmanuel Peter
Wait-so you’re telling me that 78% of people on lipophilic statins report muscle pain, but only 42% on hydrophilic? That’s a 36% difference. And you’re saying it’s not about solubility? Then what’s the mechanism? Are you just dismissing the data because it doesn’t fit your narrative? This isn’t ‘it’s complicated’-it’s statistical. If 15 million patients show a trend, you don’t get to call it ‘anecdotal’ just because rosuvastatin broke the pattern. That’s bad science.
Ollie Newland
Look, the whole hydrophilic vs lipophilic thing is a red herring. The real issue is dose intensity and polypharmacy. Rosuvastatin 20mg is a beast-it’s not the solubility, it’s the plasma concentration. Simvastatin 80mg? That’s a suicide bomber in a pharmacy. But atorvastatin 10mg? Low-dose, moderate potency, decent safety. It’s not about fat or water-it’s about exposure. And if you’re on a beta-blocker, a PPI, and a statin? You’re playing Russian roulette with your myocytes. Pravastatin’s the safest bet for the polypharmacy crowd. But if you’re 45, healthy, and need LDL down to 50? Go hard with rosuvastatin. Just monitor.