Macrolide Antibiotic Risk Calculator
This calculator estimates your risk of QT prolongation when taking macrolide antibiotics like azithromycin, clarithromycin, or erythromycin based on key medical factors. The tool is designed to help you and your doctor make informed decisions about antibiotic choices.
When you take an antibiotic for a stubborn sinus infection or bronchitis, you probably don’t think about your heart. But for some people, common macrolide antibiotics like azithromycin and clarithromycin can trigger a dangerous heart rhythm problem called QT prolongation - and in rare cases, a life-threatening arrhythmia known as Torsades de pointes. This isn’t theoretical. It’s documented, measured, and clinically significant - especially if you have other risk factors.
What Are Macrolide Antibiotics?
Macrolide antibiotics are a group of drugs used to treat bacterial infections like pneumonia, strep throat, and skin infections. The most common ones are azithromycin (Zithromax), clarithromycin (Biaxin), and erythromycin. They’ve been around since the 1950s, and for decades, they were considered safe and effective. But over the past 20 years, evidence has piled up showing they can interfere with the heart’s electrical system.
Their main job is to stop bacteria from making proteins. But they also accidentally bind to something in your heart called the hERG potassium channel. This channel helps reset your heart’s rhythm after each beat. When it’s blocked, the heart takes longer to recover - and that delay shows up on an ECG as a longer QT interval.
Why QT Prolongation Matters
The QT interval on an ECG measures how long it takes your heart’s ventricles to recharge between beats. A normal QTc (corrected for heart rate) is under 450 ms in men and under 470 ms in women. When it stretches beyond 500 ms - or increases by more than 60 ms from your baseline - you’re at higher risk for Torsades de pointes.
Torsades de pointes isn’t just an irregular heartbeat. It’s a chaotic, twisting rhythm that can turn into ventricular fibrillation - and if not treated immediately, it causes sudden cardiac death. The good news? It’s rare. The bad news? It can happen without warning, even in people who seem perfectly healthy.
Not All Macrolides Are Created Equal
Some macrolides are riskier than others. Clarithromycin tops the list. It blocks the hERG channel strongly and also inhibits liver enzymes (CYP3A4) that break down other drugs. That means if you’re taking another medication - like a statin, antifungal, or even some blood pressure pills - clarithromycin can cause those drugs to build up in your blood, making QT prolongation worse.
Erythromycin is less potent at blocking hERG, but it causes serious stomach upset. That can lead to vomiting or diarrhea, which lowers potassium levels. Low potassium = higher arrhythmia risk. Azithromycin is often seen as the safest option because it doesn’t interfere much with liver enzymes. But don’t be fooled. A 2012 study tracking over a million prescriptions found azithromycin was linked to 2.85 extra cardiovascular deaths per 1,000 courses compared to amoxicillin - especially in the first five days of use.
The FDA and American Heart Association now classify all three as drugs with “Known Risk of Torsades de Pointes.” Clarithromycin even has a black box warning in the U.S. Azithromycin’s label warns about QT prolongation, but doesn’t carry the same level of caution - which is why it still makes up 65% of all macrolide prescriptions in the U.S.
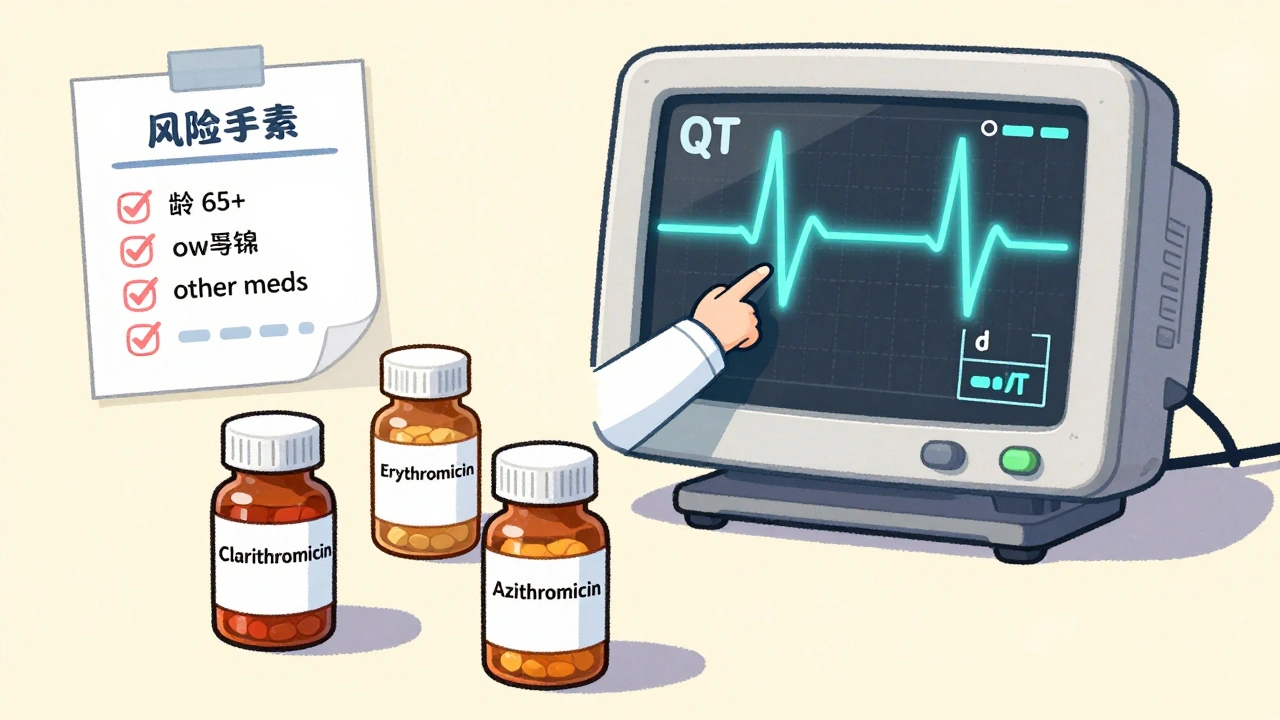
Who’s Most at Risk?
For a healthy 30-year-old with no other meds and normal heart function, the risk is very low - less than 1 in 10,000. But add just one or two risk factors, and the danger spikes.
- Female sex: 68% of TdP cases occur in women. Hormonal differences affect how the heart repolarizes.
- Age over 65: Risk doubles. Older hearts have less “repolarization reserve” - meaning less ability to compensate for channel blockage.
- Baseline QTc over 450 ms: That’s a 4.7-fold increase in risk. Many people don’t know their baseline QT because they’ve never had an ECG.
- Other QT-prolonging drugs: Taking two or more drugs that prolong QT (like antidepressants, antifungals, or antiarrhythmics) multiplies the risk. Each extra drug adds about 80% more danger.
- Low potassium or magnesium: Hypokalemia triples the risk. Diuretics, vomiting, or poor diet can cause this.
- Heart failure or structural heart disease: This increases risk more than fivefold. The heart’s already strained - adding a QT-prolonging drug is like adding fuel to a fire.
And here’s the hidden factor: some people have undiagnosed congenital long QT syndrome. Studies show 5-20% of people who develop drug-induced TdP have this inherited condition. No symptoms. No prior diagnosis. Just a genetic quirk that only shows up when they take a macrolide.
What Doctors Should Do
Guidelines from the American College of Cardiology and Infectious Diseases Society of America are clear: don’t just prescribe macrolides blindly.
- Check for risk factors before prescribing. Ask about family history of sudden death. Ask about current meds. Ask about electrolyte imbalances.
- If a patient has two or more risk factors, get a baseline ECG before starting the antibiotic.
- If the QTc is over 470 ms in men or 480 ms in women, avoid macrolides entirely. Use alternatives like doxycycline or amoxicillin.
- Recheck the ECG if the QTc increases by more than 60 ms from baseline during treatment.
- Avoid clarithromycin in patients with heart failure or those on CYP3A4-metabolized drugs.
It’s not about avoiding macrolides altogether. It’s about matching the right drug to the right patient.

What You Can Do
If you’re prescribed a macrolide antibiotic:
- Ask your doctor: “Is this the safest choice for me, given my meds and health history?”
- Know your current medications. Bring a list to your appointment - including supplements and over-the-counter drugs.
- Don’t ignore symptoms like dizziness, palpitations, fainting, or unusual fatigue while on the antibiotic.
- If you have a family history of sudden cardiac death before age 50, tell your doctor. That’s a red flag.
- Stay hydrated. Avoid excessive caffeine or alcohol while on the drug. Both can worsen electrolyte shifts.
And if you’re on azithromycin - the most commonly prescribed - don’t assume it’s harmless. The 2023 Frontiers study showed that even azithromycin can cause QT prolongation when combined with other drugs, like hydroxychloroquine. That combination was used widely during the pandemic and led to an average QTc increase of 26.2 ms - enough to push many people into danger zones.
New Tools Are Helping
Technology is catching up. In 2023, the FDA approved a handheld ECG device called CardioCare QT Monitor that gives accurate QTc readings in under 30 seconds. It’s being used in clinics and pharmacies to screen patients before prescribing macrolides.
Researchers at Brigham and Women’s Hospital developed the Macrolide Arrhythmia Risk Calculator (MARC). It uses 12 variables - age, sex, meds, ECG, kidney function, electrolytes - to predict your personal risk of TdP with 89% accuracy. It’s not in every doctor’s office yet, but it’s coming.
Future drugs may be safer. Solithromycin was designed to be a “cardiosafe” macrolide - it blocked hERG channels 78% less than clarithromycin in trials. But development stopped in 2022 because it caused liver damage. The search continues.
The Bigger Picture
Between 2010 and 2020, macrolide prescriptions in the U.S. dropped by nearly 19%. Clarithromycin use fell 23.5% after the AHA’s 2020 warning. Azithromycin remains dominant, but even its use is being scrutinized.
It’s a lesson in how a drug’s reputation can change. What was once seen as a simple, safe antibiotic is now understood as a molecule with a dual nature - powerful against bacteria, potentially dangerous to the heart. The key isn’t fear. It’s awareness.
Antibiotics save lives. But they’re not risk-free. The best outcomes happen when doctors and patients work together - asking questions, checking ECGs, and choosing wisely. Your heart might not be the first thing on your mind when you have a cough. But it’s the one organ that can’t afford to be overlooked.
Can azithromycin really cause heart problems?
Yes. While azithromycin is considered lower risk than clarithromycin or erythromycin, it still blocks the hERG potassium channel and can prolong the QT interval. Large studies, including one from 2012 tracking over 1.3 million prescriptions, found azithromycin was linked to a small but real increase in cardiovascular death - especially in the first five days of use. The risk is low in healthy people, but it becomes significant if you have other heart conditions, take other QT-prolonging drugs, or have low potassium.
Is clarithromycin safer than erythromycin?
No. Clarithromycin is actually riskier. It blocks the hERG channel more strongly than erythromycin and also inhibits liver enzymes that break down other medications. This means it can cause dangerous drug interactions that raise levels of other QT-prolonging drugs in your blood. Erythromycin causes more stomach upset, which can lead to low potassium - another risk factor. Both are risky, but clarithromycin has a higher direct effect on the heart’s electrical system.
Should I get an ECG before taking a macrolide antibiotic?
If you have two or more risk factors - such as being over 65, taking other heart or psychiatric meds, having low potassium, or a history of heart disease - yes. A baseline ECG is recommended by the American College of Cardiology. It’s quick, non-invasive, and can prevent a dangerous event. Even if you feel fine, an ECG can reveal a hidden long QT interval you didn’t know about.
What are the signs of a dangerous heart rhythm from macrolides?
Symptoms of Torsades de pointes include sudden dizziness, lightheadedness, palpitations (fluttering or racing heart), fainting, or seizures. These usually happen within the first few days of starting the antibiotic. If you experience any of these, stop the medication and seek emergency care immediately. Don’t wait. This is a medical emergency.
Are there safer alternatives to macrolide antibiotics?
Yes. For many infections, alternatives like amoxicillin, doxycycline, or cephalexin are just as effective and carry no QT prolongation risk. Your doctor should consider these first if you have heart conditions, are over 65, or are on other medications that affect heart rhythm. Antibiotic choice should be based on your full health profile - not just convenience or habit.
Can I take macrolides if I have a family history of sudden cardiac death?
Proceed with extreme caution. A family history of sudden cardiac death under age 50 could indicate an inherited long QT syndrome - even if you’ve never had symptoms. In this case, macrolides could trigger a fatal arrhythmia. Genetic testing may be recommended, but in the meantime, avoid macrolides unless absolutely necessary. Use an alternative antibiotic and consult a cardiologist.


8 Comments
Kaitlynn nail
It’s wild how we treat antibiotics like candy. We pop ‘em like gummy bears without thinking about the symphony of ions in our hearts. hERG channels? QT intervals? We’re all just one azithromycin prescription away from becoming a cautionary tale in a medical journal. 🤷♀️
Ben Greening
The clinical data presented here is both compelling and underappreciated in primary care settings. While macrolides remain convenient for common infections, the cumulative risk profile-particularly in polypharmacy patients-demands systematic ECG screening protocols. This is not alarmism; it is evidence-based prudence.
Queenie Chan
It’s like your body’s a nightclub and azithromycin is the bouncer who accidentally kicks out the potassium bouncers too. One minute you’re vibing with your sinus infection, next thing you know-boom-your heart’s doing the cha-cha with Torsades. 🎵🫀
And don’t even get me started on how we ignore baseline ECGs like they’re old voicemails. My grandma’s QTc was 492 and she thought ‘long QT’ was a new yoga pose.
David Palmer
So you’re telling me the same drug that cures my cough might kill me? Cool. I’ll just take ibuprofen and hope for the best. 😂
Also, why is azithromycin still everywhere if it’s dangerous? Because Big Pharma doesn’t care if you die slow. They care if you keep buying.
Jimmy Kärnfeldt
This post hit me right in the chest-literally. I’ve been on azithromycin twice in the last year for bronchitis and never thought twice about it. But now I’m realizing how much we trust pills without asking how they work inside us.
It’s not about fear-it’s about curiosity. Maybe we need to start treating our hearts like the fragile, beautiful machines they are. A quick ECG isn’t a hassle-it’s a gift to your future self. Thank you for writing this. I’m going to ask my doctor for a baseline next time.
Ariel Nichole
Love this breakdown. I’m a nurse and I’ve seen patients come in dizzy after finishing azithromycin and just shrug it off like it’s normal. We need way more education-not just for docs, but for patients too.
Also, the MARC calculator sounds like something we should push to every ER and urgent care. Simple, smart, lifesaving. Kudos to the researchers.
john damon
OMG I JUST TOOK AZITHROMYCIN YESTERDAY 😱 I’M GONNA DIE 😭❤️🩹
jk but also?? Like… should I be panicking?? 😅
Also my grandma had a pacemaker and she says ‘if your heart skips, just slap it’… is that valid?? 🤔
matthew dendle
so u wanna scare ppl with some fancy terms like hERG and QTc? lol
most people who get these antibiotics arent even 65 and have no heart probs. u think ur gonna die from a zpack? nah u gonna be fine
and dont even get me started on the ‘get an ecg’ crowd. its 2024 and u wanna make everyone get a test for a 1 in 10k chance? that’s not medicine thats fearmongering with a lab coat
btw clarithromycin is worse? yeah but no one takes it anymore cause it wrecks your stomach. so ur whole arg is moot