Anxiety and Depression Assessment for KS Patients
This assessment helps you understand your anxiety and depression symptoms. It is not a diagnosis but a tool to identify if you should seek professional help. Your responses will remain private.
Quick Summary
- Kaposi Sarcoma (KS) is a virus‑linked cancer that often co‑exists with HIV/AIDS.
- Living with KS can trigger anxiety and depression due to visible lesions, treatment side‑effects, and stigma.
- Recognize key emotional signs early - racing thoughts, persistent sadness, sleep changes, loss of interest.
- Practical tools include mindfulness breathing, gentle exercise, structured therapy, medication, and peer support.
- Seek professional help when symptoms interfere with daily life or when you notice worsening mood.
- Focus on managing Kaposi Sarcoma anxiety alongside physical treatment.
Understanding Kaposi Sarcoma
Kaposi Sarcoma is a vascular cancer caused by human herpesvirus‑8 (HHV‑8) that frequently appears in people with weakened immune systems, especially those living with HIV/AIDS. It shows up as reddish‑purple patches on the skin, mucous membranes, or internal organs. While antiretroviral therapy (ART) has reduced its incidence, KS remains a chronic reality for many patients, requiring ongoing monitoring and occasional chemotherapy or radiation.
The disease’s physical visibility often fuels self‑consciousness, and the need for regular doctor visits can feel overwhelming. Understanding the medical backdrop helps us separate what can be treated medically from what needs emotional care.
How KS Impacts Mental Health
When you add a cancer diagnosis to an existing HIV status, the brain’s stress response goes into overdrive. The body releases cortisol, a hormone that, in excess, can exacerbate both anxiety and depressive moods. Moreover, HIV/AIDS itself carries a heavy social stigma that can amplify feelings of isolation.
Studies from 2023-2024 show that up to 45% of KS patients report clinically significant anxiety, while 38% experience moderate to severe depression. These numbers are higher than in the general cancer population, underscoring the need for targeted mental‑health strategies.
Spotting Anxiety and Depression Early
Recognizing emotional shifts early can prevent a slide into chronic distress. Common anxiety signals include:
- Racing thoughts about disease progression or treatment side‑effects.
- Physical tension - clenched jaws, shaky hands, rapid heartbeat.
- Sleep disturbances, especially difficulty falling asleep.
Depression often shows up as:
- Persistent low mood or a sense of hopelessness.
- Loss of interest in activities that once brought joy.
- Changes in appetite, energy, or concentration.
If you notice any of these patterns lasting more than two weeks, it’s a cue to act.
Managing Anxiety: Practical Tools
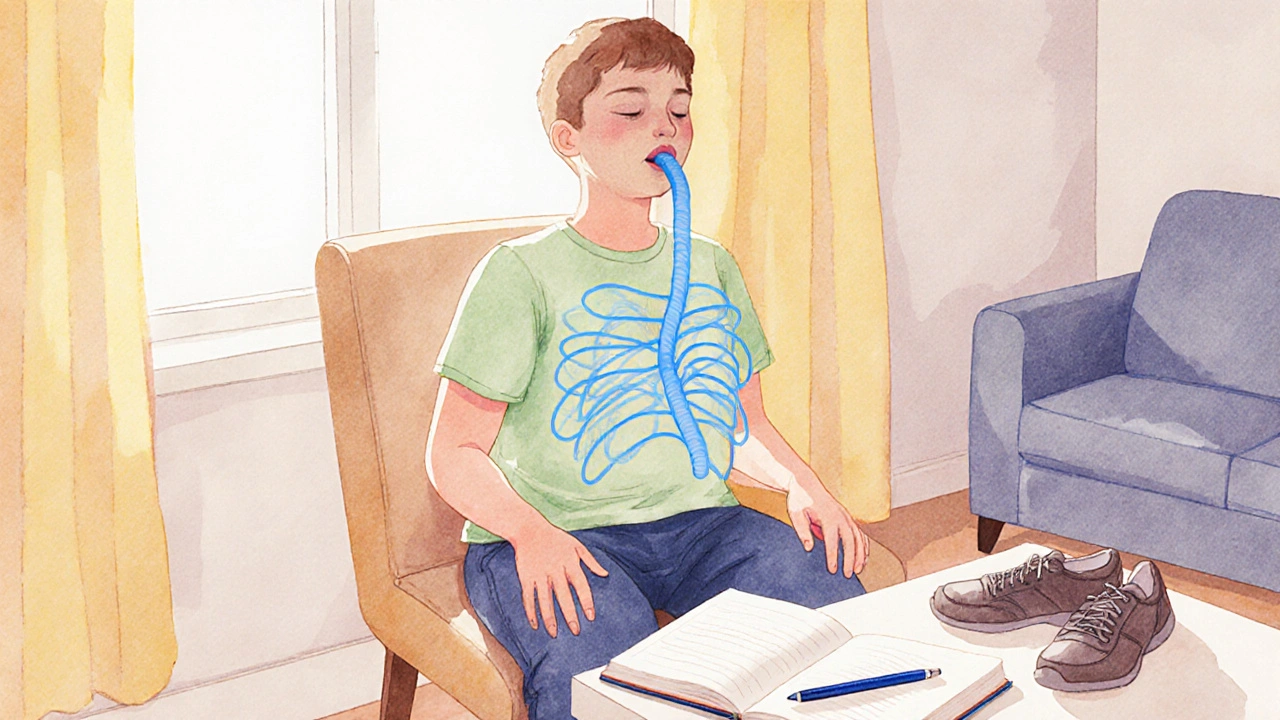
Anxiety can feel like a never‑ending loop, but simple, evidence‑based practices break the cycle. Here are five steps you can start today:
- Grounding breaths: Inhale for a count of four, hold two seconds, exhale for six. Repeat five times. This reduces cortisol spikes within minutes.
- Progressive muscle relaxation: Tense each muscle group for three seconds, then release. Works especially before medical appointments.
- Mindful journaling: Write down worries for five minutes, then list three concrete actions you can take. The act of externalizing thoughts lowers their grip.
- Physical activity: Even a 15‑minute walk boosts endorphins and improves sleep quality.
- Therapeutic dialogue: Psychotherapy, especially cognitive‑behavioral therapy (CBT), equips you with coping scripts tailored to health‑related fears.
If anxiety becomes disabling, talk to your doctor about short‑term antidepressants that also treat anxiety (e.g., sertraline or escitalopram). These medications are safe alongside most antiretroviral regimens.
Managing Depression: Practical Tools
Depression often hides behind fatigue and lack of motivation. Tackling it requires a blend of lifestyle tweaks and, when needed, medical support.
- Structured daily routine: Set regular wake‑up, meal, and bedtime slots. Predictability combats the “nothing matters” feeling.
- Activity scheduling: Plan just one enjoyable activity each day - a favorite podcast, a short craft, or a video call with a friend.
- Light exposure: Get 20 minutes of natural sunlight each morning. It regulates serotonin and improves mood.
- Social connection: Join a support group for KS or HIV patients. Sharing experiences reduces isolation.
- Professional therapy: Interpersonal therapy (IPT) focuses on relationship challenges that often worsen depression.
- Medication review: If symptoms persist, a psychiatrist may prescribe a selective serotonin reuptake inhibitor (SSRI) compatible with your antiretroviral therapy plan.

Building a Support System
You don’t have to face KS and its emotional fallout alone. A robust support network can be a lifesaver.
- Family & friends: Educate them about KS and its mental‑health implications. Simple statements like “I feel anxious when I think about my skin lesions” open the door for empathy.
- Healthcare team: Ask your oncologist and HIV specialist to screen for mood disorders at each visit. Many clinics now have embedded mental‑health counselors.
- Online communities: Forums such as the International Kaposi Sarcoma Alliance provide peer‑to‑peer advice and coping stories.
- Spiritual or cultural groups: If faith or cultural practice is important, integrating those rituals can add meaning and reduce distress.
Documenting who you can call in a crisis (e.g., a trusted friend, therapist, or a 24‑hour helpline) reduces panic when symptoms spike.
When to Seek Professional Help
Knowing when self‑management isn’t enough is key. Seek a mental‑health professional if you:
- Feel hopeless or consider self‑harm.
- Experience panic attacks that impair daily functioning.
- Notice a sudden decline in medication adherence because of low mood.
- Observe worsening sleep, appetite, or weight loss despite lifestyle tweaks.
Many hospitals now offer integrated oncology‑psychiatry clinics, reducing the need for separate appointments. Ask your primary HIV‑care provider for a referral.
Quick Checklist for Daily Mental‑Health Maintenance
| Action | Why it matters | Time needed |
|---|---|---|
| Grounding breath exercise (5 min) | Lowers cortisol, eases racing thoughts | 5 minutes |
| Morning sunlight exposure | Boosts serotonin, regulates circadian rhythm | 15-20 minutes |
| One pleasant activity (e.g., call a friend) | Counteracts anhedonia, builds social connection | 30 minutes |
| Journal worries & create action steps | Externalizes anxiety, creates plan | 10 minutes |
| Check‑in with therapist or support group (weekly) | Professional guidance, peer validation | Varies |
Frequently Asked Questions
Can Kaposi Sarcoma cause depression on its own?
KS itself doesn’t produce chemicals that cause depression, but the disease’s visible lesions, treatment side‑effects, and the underlying immune suppression create chronic stress, which can trigger depressive episodes.
Is it safe to take antidepressants while on antiretroviral therapy?
Most SSRIs, such as sertraline and fluoxetine, have been studied alongside common ART regimens and show minimal interaction. Always discuss dosage with your HIV specialist before starting any new medication.
Do support groups really help with anxiety?
Yes. Peer groups provide validation, practical tips, and a sense of belonging. A 2022 survey of 312 KS patients found a 27% reduction in self‑reported anxiety scores after regular group participation for three months.
What lifestyle changes lower the risk of mood swings?
Consistent sleep, balanced nutrition (especially omega‑3 rich foods), daily light exposure, and limiting alcohol or stimulants help stabilize mood. Pair these with a regular exercise routine for best results.
How often should I be screened for depression?
Screening every three to six months is advisable for KS patients, especially after a flare‑up or a change in treatment. Use validated tools like the PHQ‑9 during clinic visits.


13 Comments
Rahul yadav
Seeing a tool like this for KS patients really hits home. I’ve known a friend battling Kaposi who constantly worries about the next flare‑up 😔. It’s amazing how simple check‑boxes can open up a conversation with doctors about mental health. The emojis help remind us that it’s okay to feel scared, and that seeking help is a sign of strength 😊.
Dan McHugh
Interesting approach.
Sam Moss
Let me break down why this kind of assessment matters for anyone dealing with Kaposi sarcoma, especially when anxiety and depression creep in. First, the mind and body are tightly linked; chronic illness can be a constant source of stress that fuels a vicious cycle of worry and fatigue. Second, early detection of mental health symptoms can prevent them from escalating to severe depression or even suicidal ideation, which unfortunately isn’t rare in long‑term disease management. Third, the questionnaire’s design, using clear, non‑technical language, lowers the barrier for patients who might feel overwhelmed by medical jargon. Fourth, having a private, self‑administered tool empowers patients to take ownership of their mental health without feeling judged. Fifth, clinicians can use the results to tailor interventions-whether that’s a referral to a therapist, prescribing low‑dose antidepressants, or simply scheduling more frequent check‑ins. Sixth, the inclusion of physical tension and sleep disturbances captures a broader symptom picture, because anxiety often manifests somatically. Seventh, the tool’s digital format makes it easy to integrate into telehealth visits, a growing necessity in the post‑COVID era. Eighth, it respects patient confidentiality, which is crucial when dealing with a stigmatized condition like KS. Ninth, by normalizing mental health screening, we reduce the shame that often keeps patients silent. Tenth, it can serve as a data point for researchers tracking the psychosocial burden of KS across populations. Eleventh, the straightforward scoring system helps both patients and providers quickly see where the biggest concerns lie. Twelfth, it encourages patients to reflect on their daily experiences, fostering self‑awareness. Thirteenth, it may uncover hidden issues like changes in appetite or concentration that affect treatment adherence. Fourteenth, the prompt about panic attacks can flag acute episodes that need immediate attention. Fifteenth, the overall design embodies a compassionate, patient‑centered approach that can improve overall quality of life. In short, tools like this are not just check‑boxes; they’re lifelines for navigating the emotional turbulence that comes with chronic disease.
Suzy Stewart
Great points, Rahul! 🙌 It’s vital to remember that mental health tools shouldn’t replace professional care, but they’re a solid first step. The emojis you added really humanize the experience, and the reminder that reaching out is a strength is spot‑on. Keep spreading awareness! 🌟
Traven West
Finally, a questionnaire that actually looks decent-no endless drivel. The language is crisp and the layout isn’t a nightmare. Though, “Do you feel hopeless?” is a bit melodramatic, but I guess it’s necessary.
Jonny Arruda
Cool tool, seems straightforward enough. Might help folks who otherwise ignore the mental side.
Melissa Young
Look, this is how we should be handling KS patients in the West-no fluff, straight to the point, with actionable steps. If you’re not using an assessment like this, you’re basically ignoring a huge part of the disease burden. Get it done.
Jennifer Ramos
Thanks for sharing! I love how the assessment encourages a conversation with healthcare providers. It’s a collaborative effort, and the gentle language makes it feel supportive. 🌈
Amy Collins
Meh, looks decent but could use more visuals. Anyway, nice effort.
amanda luize
This looks pretty legit on the surface, but have you considered that the pharma industry might be pushing these tools to funnel more patients into their drug pipelines? The phrasing “consider therapy” could be a subtle nudge toward patented meds. Just saying.
Chris Morgan
While the assessment seems thorough, it neglects the socioeconomic factors that exacerbate mental health issues in KS patients. Ignoring these variables limits its effectiveness.
Pallavi G
Hi everyone! As someone who’s been involved in patient education, I think this tool is a solid starting point. It’s clear, concise, and respects patient privacy. Adding a brief guide on how to discuss results with a doctor would make it even better. Keep it up! ✨
Rafael Lopez
Excellent initiative! The assessment covers the key psychological domains-anxiety, depression, sleep, and somatic tension. It would be great to see integration with electronic health records for seamless follow‑up. Also, a printable version could help patients without reliable internet access. Well done!!!