When you pick up a prescription, you might assume the pharmacist will give you the cheapest option - but that’s not true everywhere. In some states, pharmacists must swap your brand-name drug for a generic. In others, they can only do it if you say yes. These rules aren’t random. They’re written into state law, and they directly affect how much you pay, whether you stick with your treatment, and even how safe your meds are.
What’s the Difference Between Mandatory and Permissive Substitution?
Mandatory substitution means the pharmacist has to give you the generic version - unless your doctor specifically says not to. Think of it like a default setting: if nothing stops it, the switch happens. Permissive substitution is different. Here, the pharmacist can swap the drug, but they don’t have to. They decide based on their judgment, your preferences, or whether you give permission.
This isn’t just a technicality. It changes behavior. In states with mandatory rules, generic drugs are filled far more often. A 2011 study found that six months after a brand-name drug lost its patent, generics were used in 48.7% of prescriptions in mandatory states. In permissive states? Just 30%. That’s nearly a 20-point gap. And it’s not just about money - it’s about access. If you’re on Medicaid or can’t afford your meds, this difference can mean skipping doses or stopping treatment altogether.
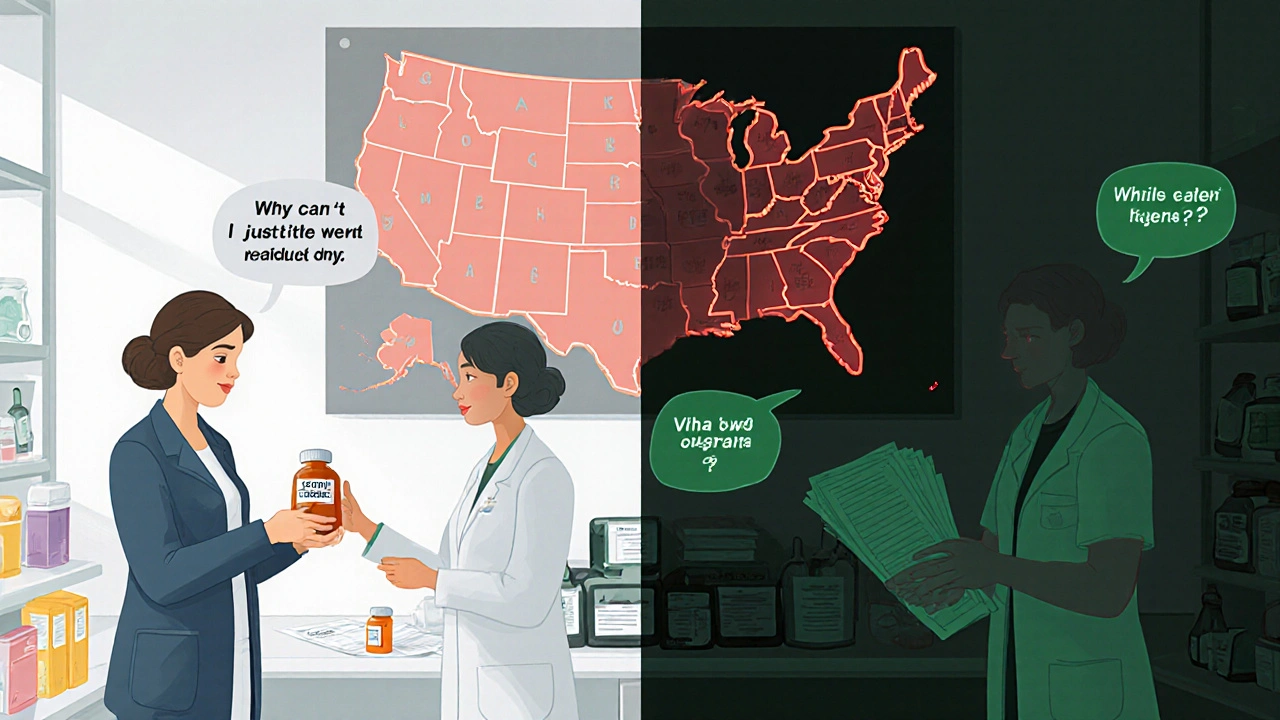
Which States Require Substitution? (And Which Don’t)
As of 2020, 19 states - including Alabama, Alaska, Arizona, Colorado, Connecticut, Indiana, Kentucky, Maine, Maryland, Massachusetts, Mississippi, Montana, New Hampshire, North Dakota, West Virginia, and others - require pharmacists to substitute generics unless the prescriber blocks it. These are mandatory substitution states.
The rest are permissive. That includes big states like California, Florida, Illinois, Michigan, New York, and Texas - but don’t assume they’re all the same. Even in permissive states, rules vary. Some require you to sign a form. Others make the pharmacist call you first. A few even require the pharmacist to explain why they’re not substituting. It’s messy, and it’s confusing for patients.
There’s also a growing gap between small-molecule drugs and biologics. For things like insulin or rheumatoid arthritis drugs, which are made from living cells, 45 states have stricter rules. Even if a biosimilar (the generic version of a biologic) is approved, pharmacists often can’t swap it without the doctor’s explicit okay. That’s because of fears about immune reactions when switching between products - even if science says it’s safe.
The Hidden Rules: Consent, Notification, and Liability
It’s not just about whether substitution is mandatory or optional. There are four key layers that make each state’s law unique:
- Duty to substitute: Must they do it? Or can they choose?
- Notification: Do they have to tell you in writing - separate from the pill bottle - that you got a generic?
- Consent: Do you have to say yes before they swap it?
- Liability: If something goes wrong after the switch, are they protected?
Thirty-one states and Washington, D.C., require pharmacists to notify you - even if you already know you’re getting a generic. Seven states plus D.C. require your explicit consent. That means if you don’t sign a form or verbally agree, they can’t substitute. And here’s the kicker: in those states, generic use dropped to just 32.1% after patent expiration. In states with no consent rule? It hit 98.1%.
Then there’s liability. Twenty-four states don’t protect pharmacists from lawsuits if a patient has a bad reaction after a generic is swapped. That means pharmacists in those states are more likely to avoid substitution - even if it’s allowed - just to stay safe. So a rule meant to save money ends up blocking access.
How Prescribers Block Substitution - And Why It Matters
Your doctor can stop substitution by writing “Dispense as Written” or “Brand Medically Necessary” on your prescription. But how they do it depends on your state. In some places, prescriptions have two lines - one for the brand, one for the generic. If they sign the brand line, substitution is blocked. In others, they have to write out the phrase by hand.
But here’s the problem: not all doctors know the rules. And some patients don’t realize they’re being denied a cheaper option. A study found that pharmacists in mandatory states with consent requirements were almost twice as likely to avoid substituting narrow therapeutic index drugs - like blood thinners or epilepsy meds - even when it was medically appropriate. Why? Because they’re scared of liability or getting it wrong.
Why This Matters for Your Health and Wallet
Generic drugs cost 80-85% less than brand-name versions. That’s not a small savings. The Congressional Budget Office estimated that raising generic use by just 1% would save Medicare Part D $160 million a year. Multiply that across Medicaid, private insurers, and out-of-pocket patients - and you’re talking billions.
But money isn’t the only issue. When people can’t afford their meds, they skip doses. That leads to hospital visits, worse outcomes, and higher long-term costs. A 2020 JAMA study found that states with fewer barriers to substitution had better medication adherence. The authors called it “an important lever” to improve health and cut spending.
For patients on chronic meds - diabetes, high blood pressure, depression - switching to a generic isn’t just about cost. It’s about stability. If you’re getting the same active ingredient, why shouldn’t you get the cheaper version? The answer, in too many places, is bureaucracy, not science.
The Biologics Problem: Why the Rules Are Tighter
Biosimilars are the generics of complex biologic drugs. They’re not exact copies - they’re highly similar. That’s why states treat them differently. While small-molecule generics can be swapped easily, biosimilars often require extra steps: doctor approval, patient notification, recordkeeping, and sometimes even a new prescription.
Only nine states and D.C. treat biosimilars the same as regular generics. The rest have layered rules. Why? Fear. Some doctors worry that switching between biologics could trigger immune reactions. While the FDA says they’re safe, the legal system hasn’t caught up. So pharmacists hesitate. Patients pay more. And progress slows.
What You Can Do
You don’t have to accept whatever your pharmacist gives you. Ask:
- “Is there a generic version available?”
- “Do I need to sign anything to get it?”
- “Why am I getting the brand-name drug?”
If you’re being charged more and you don’t know why, contact your state board of pharmacy. They track these laws. You might find your state has a mandatory substitution rule - and your pharmacist is ignoring it.
Also, talk to your doctor. If they wrote “Dispense as Written,” ask why. Is it because of safety? Or because they’re not aware of the generic? Many doctors still think generics are inferior - even though the FDA says they’re just as safe and effective.
Where the System Is Changing
The number of mandatory substitution states rose from 14 in 2014 to 19 in 2020. That’s a trend toward more cost-saving policies. But the rise of biosimilars and specialty drugs is forcing new debates. Some states are trying to simplify rules. Others are adding more restrictions.
What’s clear is this: the patchwork of state laws isn’t working well. Patients get different treatment depending on where they live. Pharmacists are stuck in legal gray zones. And the system isn’t optimized for health - it’s optimized for paperwork.
Real reform means making substitution the default - without unnecessary consent forms, without fear of lawsuits, and without confusing rules that stop people from getting the meds they need. Until then, knowing your state’s law is your best tool to save money and stay healthy.
Can my pharmacist substitute my brand-name drug without telling me?
In most states, no. Thirty-one states and Washington, D.C., require pharmacists to notify you separately - even if the pill bottle says it’s generic. Some states also require your written or verbal consent before making the switch. Always check your state’s rules - or ask your pharmacist directly.
Why do some states require patient consent for generic substitution?
Some states added consent rules out of concern that patients might not understand generics are safe. But research shows these rules backfire. States requiring consent saw generic use drop to just 32.1%, compared to 98.1% in states without consent. The extra step creates friction - and patients often don’t know they’re being denied a cheaper, equally effective option.
Are biosimilars treated the same as regular generics under state law?
No. Forty-five states have stricter rules for biosimilars - the generic versions of complex biologic drugs like insulin or rheumatoid arthritis treatments. Many require doctor approval, patient notification, or recordkeeping. Only nine states and D.C. treat them the same as small-molecule generics. This reflects lingering safety concerns, even though the FDA has approved them as safe and effective.
What does "Dispense as Written" mean on my prescription?
It means your doctor has asked the pharmacist not to substitute a generic version. This phrase overrides state substitution laws. But it’s not always necessary. Many doctors use it out of habit, not medical need. Ask if it’s truly required - especially if you’re paying more.
Can I be held liable if I take a generic drug and have a bad reaction?
No. Patients are not liable for adverse reactions to generic drugs. Liability falls on the manufacturer or, in rare cases, the pharmacist - but only if they violated state law or acted negligently. The FDA requires generics to meet the same safety and effectiveness standards as brand-name drugs. If you’re concerned, talk to your doctor or pharmacist before switching.
Do all states use the FDA’s Orange Book to decide which generics can be substituted?
Most do. The FDA’s Orange Book lists drugs that are therapeutically equivalent - meaning they work the same way. But a few states allow substitution beyond that list, while others restrict it further. Always check your state’s pharmacy board website for the exact rules - they may have their own formulary or restrictions.
What’s Next for Generic Drug Laws?
The trend is clear: more states are moving toward mandatory substitution. But as drugs get more complex - especially with biosimilars, combination therapies, and personalized medicine - the rules need to evolve too. The goal shouldn’t be to block substitution. It should be to make it safe, simple, and automatic - unless there’s a real medical reason not to.
If you’re paying full price for a drug that has a generic, ask why. You might be surprised at the answer - and what you can do about it.

12 Comments
Conor McNamara
so i been thinkin… what if the big pharma companies are secretly paying off state lawmakers to keep the permissive rules? i mean, why else would california and texas still make us sign forms just to get a $3 generic? they dont want us healthy, they want us hooked on $500 pills. and dont even get me started on how the pharmacists get paid more to push brand names… its all rigged.
Leilani O'Neill
How utterly predictable. The American healthcare system remains a grotesque parody of efficiency, where bureaucratic inertia and misplaced patient autonomy trump evidence-based policy. Mandatory substitution isn't just prudent-it's a moral imperative. The fact that 19 states still allow this archaic consent theater is a national disgrace. If you can't trust a pharmacist to dispense a bioequivalent generic, you shouldn't be allowed to leave the house.
Riohlo (Or Rio) Marie
Oh honey, let me tell you-this isn’t about drugs, it’s about power. The pharma lobby doesn’t want you to know that generics are just as good because then they’d lose their monopoly on your suffering. And don’t even get me started on how they’ve weaponized ‘safety concerns’ around biosimilars to keep prices sky-high. It’s not science-it’s a financial heist wrapped in white coats and legalese. You think your doctor’s ‘Dispense as Written’ note is medical advice? Nah. That’s a corporate directive printed on a napkin at a golf retreat.
And the consent forms? Please. That’s not patient empowerment-that’s a psychological trap. They make you feel like you’re in control while actually making you jump through hoops so the system can profit off your confusion. I’ve seen elderly people skip meds because they didn’t understand the paperwork. That’s not healthcare. That’s cruelty with a pharmacy stamp.
steffi walsh
This is actually really helpful and I’m so glad someone laid it out clearly! I had no idea my state required consent forms-I thought I was just being extra cautious when I asked my pharmacist. But now I know I have the right to ask for the generic and not feel guilty about it. Thank you for giving me the courage to speak up. You’re right-our health shouldn’t depend on where we live or how much paperwork we can handle. 💪
Kristina Williams
they’re lying. the generics are made in china and filled with rat poison. i read it on a forum. my cousin’s neighbor’s dog got sick after taking a generic and now it can’t walk. they don’t tell you this. the fda is in on it. you think they care about you? they care about money. i only take brand name now. even if it costs my rent.
Shilpi Tiwari
From a pharmacoeconomic standpoint, the variance in substitution statutes creates significant therapeutic inertia, particularly in narrow therapeutic index (NTI) drugs. The heterogeneity in state-level liability protections introduces non-clinical variables into therapeutic decision-making, thereby undermining the principle of equivalence enshrined in the FDA’s AB-rating system. The absence of federal preemption exacerbates regulatory arbitrage, enabling pharmaceutical manufacturers to exploit jurisdictional fragmentation to maintain price premiums.
Christine Eslinger
I’ve worked in community pharmacy for 18 years, and I can tell you this: the people who suffer the most from these patchwork laws are the elderly, the low-income, and the chronically ill. I’ve watched patients cry because they couldn’t afford their insulin-and then I had to explain that yes, there’s a biosimilar, but I can’t give it to them unless the doctor rewrites the script, and the patient signs three forms, and the insurance approves it, and the pharmacy has to log it in triplicate. It’s not about safety. It’s about systems that don’t care if you live or die, as long as the paperwork is perfect.
Change doesn’t come from laws. It comes from people asking, ‘Why?’ And then refusing to accept the answer. You’re not being difficult. You’re being smart.
Denny Sucipto
Man, I used to think generics were sketchy too-until my knee started acting up and I was paying $200 for a brand-name NSAID. I asked for the generic. Saved me $180 a month. No difference in how I felt. Zero. Not a single side effect. My doctor was shocked I even knew generics existed. Turned out he was just used to writing ‘DAW’ out of habit. I told him to stop. Now he does. You don’t need permission to save your own money. Just ask.
Holly Powell
The entire premise of this article is dangerously naive. You assume pharmacists are neutral actors in a rational market. They’re not. They’re profit-driven gatekeepers embedded in a broken system. And the idea that patients are ‘empowered’ by consent forms? That’s victim-blaming dressed up as consumer choice. The real issue isn’t the law-it’s the total absence of federal oversight. Letting 50 states decide drug access is like letting 50 people pick your heart medication based on their lunch preferences.
Emanuel Jalba
THIS IS WHY WE CAN’T HAVE NICE THINGS!!! 🤬 I just got my blood pressure med switched and now I feel like I’m being slowly poisoned by a Chinese factory worker who hates Americans!! 🇺🇸💀 I told my pharmacist, ‘I didn’t sign anything!’ and he just shrugged! This is a CONSPIRACY. Someone is replacing my meds with CRACK!! 😭 I’m calling the FBI. And my senator. And my yoga instructor. THIS ENDS NOW. #GenericGate #PharmaIsEvil
Heidi R
You’re all missing the point. The real problem is that pharmacists are being used as pawns in a system designed to keep you dependent. They don’t want to be the ones making the call. So they hide behind consent forms and liability fears. But the truth? They’re scared of you. They know you’re smarter than they think. And that terrifies them.
Christine Eslinger
Christine Eslinger: I’ve seen this too. One time, a woman came in crying because her pharmacist refused to switch her antidepressant to a generic-said she ‘had to sign a form’ even though her state didn’t require it. I checked the law. He was lying. I called the state board. He got a warning. She got her generic the next day. Sometimes, the system breaks when someone just asks.
And to the person above me-yes. They’re scared. Not of lawsuits. Of being exposed as part of a broken machine. That’s why they hide behind rules. Don’t let them.