MAOI-Opioid Safety Checker
Check Opioid Safety with MAOIs
Select an opioid to see if it's safe to use with MAOIs (like Nardil, Parnate, or Marplan). This tool is based on FDA guidelines and clinical evidence.
Combining opioids with monoamine oxidase inhibitors (MAOIs) isn't just risky-it can kill. This isn’t theoretical. People have died from this mix, sometimes within hours of taking both drugs. If you're on an MAOI for depression, or someone you care about is, hearing this might feel shocking. But it’s real, and it happens more often than you think.
Why This Combination Is So Dangerous
MAOIs like phenelzine (Nardil), tranylcypromine (Parnate), and isocarboxazid (Marplan) work by blocking enzymes that break down brain chemicals like serotonin, norepinephrine, and dopamine. That’s how they help with depression. But when you add certain opioids, you’re pouring gasoline on a fire. Some opioids don’t just relieve pain-they also flood your system with serotonin. Tramadol, meperidine (Demerol), methadone, and even dextromethorphan (found in cough syrups) do this. When MAOIs are already preventing serotonin from being cleared, these opioids push levels into dangerous territory. That’s how serotonin syndrome starts: a runaway buildup of serotonin that causes your body to overheat, your muscles to lock up, and your nervous system to go haywire. Symptoms show up fast-sometimes within an hour. High fever (104°F+), stiff muscles, confusion, seizures, rapid heartbeat, and high blood pressure. In severe cases, it leads to organ failure. A 2019 review found that 2-12% of people who develop severe serotonin syndrome die from it. And this isn’t rare. The FDA’s own database recorded 89 deaths from MAOI-opioid combinations between 2015 and 2022.The Opioids That Are Most Dangerous
Not all opioids are equally risky. Some are outright banned when you’re on an MAOI. Others are risky enough that doctors avoid them unless there’s no alternative.- Meperidine (Demerol): The worst offender. Over 37 deaths were documented between 1960 and 2010. It doesn’t just increase serotonin-it releases it directly. The FDA, American Psychiatric Association, and WHO all say: never use this with MAOIs.
- Tramadol: Often mistaken as a "safe" painkiller because it’s not a traditional opioid. But it inhibits serotonin reuptake as strongly as some antidepressants. Over 68 cases of serotonin syndrome were linked to tramadol + MAOIs between 2010 and 2022. It’s responsible for more than half of all documented cases.
- Methadone: Used for pain and addiction treatment. It has multiple ways of interfering with serotonin and norepinephrine. Even though it’s less dangerous than meperidine, it still carries a significant risk.
- Dextromethorphan: Found in over-the-counter cough meds. People don’t realize it’s an opioid-like substance. A single dose can trigger a reaction in someone on an MAOI.
Even "safer" opioids like morphine, oxycodone, and hydromorphone aren’t risk-free. They can still cause serotonin buildup indirectly. The safest approach? Avoid all opioids unless absolutely necessary-and even then, only under strict supervision.
The 14-Day Washout Rule
If you’re switching from an MAOI to an opioid-or vice versa-timing matters more than you think. MAOIs don’t just disappear when you stop taking them. The enzymes they block take time to regenerate. For irreversible MAOIs (the most common type), you need a 14-day waiting period after stopping the MAOI before starting any opioid with serotonergic effects. This isn’t a suggestion. It’s a hard rule backed by the FDA, Mayo Clinic, and American Society of Anesthesiologists. Why 14 days? Because that’s how long it takes for your body to rebuild enough monoamine oxidase enzyme activity to safely handle opioids. Skip this, and you’re gambling with your life. Reversible MAOIs like moclobemide (Aurorix) are slightly less risky. They clear from your system faster, so a 24-hour gap may be enough. But even then, experts recommend caution. There are documented cases of serotonin syndrome with moclobemide + tramadol at normal doses.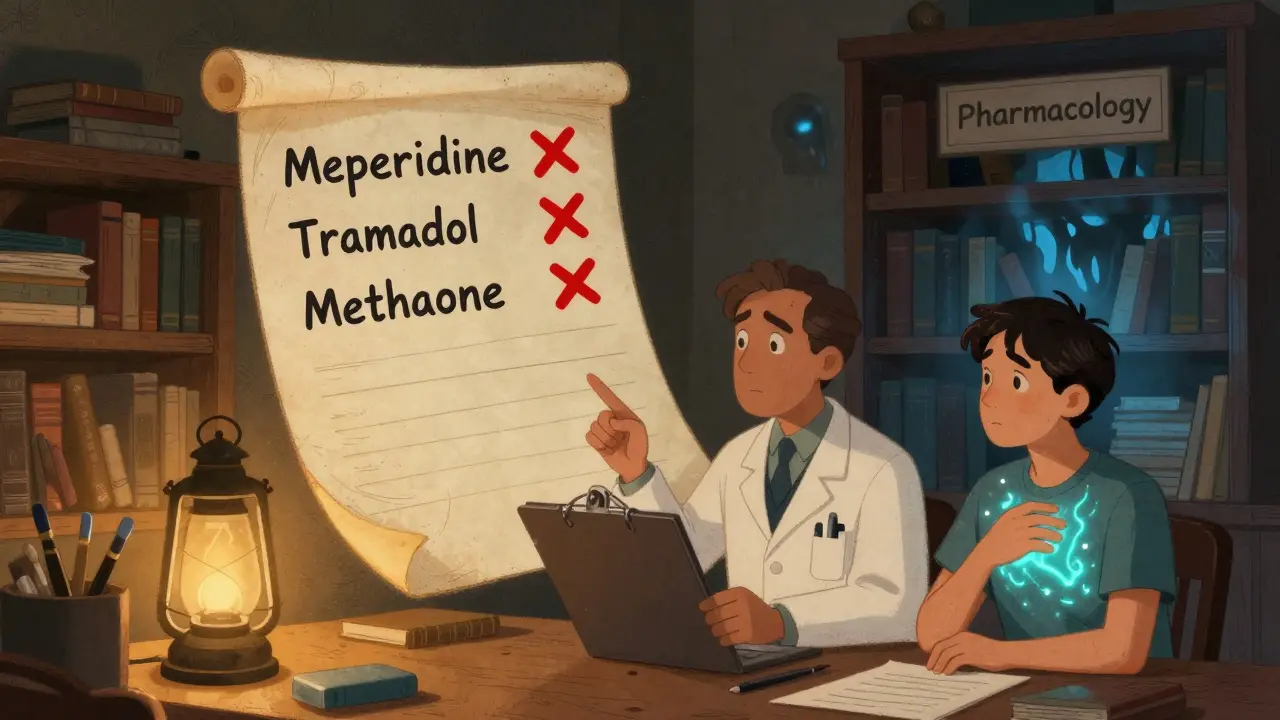
What to Use Instead
If you’re on an MAOI and need pain relief, you still have options. But you need to avoid the wrong ones.- Buprenorphine: This partial opioid agonist has minimal serotonin effects. Studies show it’s safe for acute pain in MAOI users when given at low doses (0.2-0.4 mg sublingual). It’s now the go-to choice in hospitals.
- Acetaminophen (Tylenol): Safe, effective for mild to moderate pain. No interaction risk.
- NSAIDs: Ibuprofen, naproxen, celecoxib-all fine. Just watch kidney function if you’re on long-term use.
- Non-drug options: Physical therapy, heat/cold packs, nerve blocks, acupuncture. These aren’t just alternatives-they’re often more effective long-term.
Avoid tapentadol (Nucynta), fentanyl patches, and any opioid with "serotonin" in its mechanism. Even if your doctor says "it’s okay," double-check with a pharmacist. Many prescribing errors happen because providers forget MAOIs are still active in the body.
Real Stories, Real Consequences
One Reddit user, u/ChronicPainWarrior, described being prescribed tramadol for a toothache while on phenelzine. Within hours, their body temperature hit 107.1°F. They couldn’t breathe. Their muscles seized. They spent three days in intensive care. "I thought I was getting relief," they wrote. "I didn’t know I was walking into a death trap." An anesthesiologist in a medical forum recalled two near-fatal cases. One patient on Parnate got Demerol after surgery and spiked to 240/140 blood pressure. Another, on Nardil, developed serotonin syndrome after tramadol for dental work. Both required emergency drugs, cooling blankets, and ICU monitoring. These aren’t outliers. The FDA’s database has 427 reports of MAOI-opioid reactions since 2015. And that’s just what got reported. Many cases go unrecorded because doctors don’t connect the dots.Why This Keeps Happening
You’d think this would be a solved problem by now. But it’s not. In 2022, a study found that 4.3% of MAOI users received a contraindicated opioid within 14 days of starting the MAOI. That’s over 11,000 dangerous prescriptions every year in the U.S. alone. Why?- Tramadol is still marketed as a "non-narcotic," leading patients and doctors to underestimate its danger.
- Primary care doctors-who prescribe most pain meds-are less familiar with MAOI interactions than psychiatrists.
- Patients don’t always tell their doctors they’re on an MAOI. They forget. Or they think it’s "just for depression," not a drug that affects everything else.
- Electronic health records have "hard stops," but 14% of providers still override them.
Even worse, a 2022 study found that 31% of emergency room doctors didn’t know tramadol was contraindicated with MAOIs. That’s not just a gap in knowledge-it’s a public health failure.

What You Can Do
If you’re on an MAOI:- Carry a wallet card listing all contraindicated drugs. The National Alliance on Mental Illness provides them free.
- Always tell every new doctor, dentist, or pharmacist you’re on an MAOI-even if you think they won’t prescribe opioids.
- Never take OTC cough medicine without checking the label for dextromethorphan.
- Use the 14-day washout rule religiously. No exceptions.
If you’re a prescriber:
- Check your EHR alerts. Don’t override them unless you’ve double-checked the guidelines.
- Use buprenorphine or non-opioid options first.
- Teach your patients. Many don’t know they’re at risk.
What’s Changing
Good news: things are improving. The FDA now requires updated medication guides for all MAOIs that list 12 specific contraindicated opioids. The European Medicines Agency now requires mandatory interaction training for all prescribers in EU countries. Hospitals in the U.S. have automated systems that block these prescriptions-and they’ve prevented over 8,000 dangerous combinations in 2021 alone. A new digital tool called SerotoninSafe, approved by the FDA in 2023, integrates with electronic records and cuts prescribing errors by 76%. Research is also underway into safer MAOIs-like transdermal patches that deliver lower brain concentrations-and selective MAO-B inhibitors that don’t affect serotonin at all. But the danger hasn’t disappeared. The number of MAOI users in the U.S. is still around 1.2 million. And every year, some of them get prescribed the wrong painkiller.Final Warning
This isn’t a "maybe" or a "be careful." It’s a hard line: do not combine MAOIs with tramadol, meperidine, methadone, or dextromethorphan. The risk isn’t theoretical. People have died. And it happens faster than you think. If you’re on an MAOI, your pain management plan needs to be different. Work with your doctor. Use safer alternatives. And never, ever assume a painkiller is "safe" just because it’s prescribed.One wrong choice can end a life. Don’t let it be yours.


15 Comments
Mike Hammer
Man, I never realized how many OTC meds have dextromethorphan. I’ve been taking cough syrup for years and didn’t think twice. This post literally saved my life. Thanks for laying it out so clearly.
Daniel Dover
14-day washout. Non-negotiable.
Joe Grushkin
The FDA database has 89 deaths? That’s laughable. You think that’s all? Try multiplying by ten because most ER docs don’t even document serotonin syndrome correctly. They just write 'cardiac arrest' and move on. This is systemic negligence disguised as medical practice.
Mandeep Singh
You people in the US are so careless. In India, we don’t just take random painkillers. We ask our Ayurvedic doctors first. Tramadol? It’s banned in many states here for a reason. You think your 'personal freedom' is worth dying over? Your healthcare system is a joke. I’ve seen patients on MAOIs get prescribed tramadol and then end up in ICU. No one listens. No one cares. This is why your life expectancy is dropping.
Esha Pathak
There’s a deeper truth here - we treat pain like it’s a villain to be crushed, not a signal to be heard. We reach for opioids like they’re magic bullets, ignoring the whisper of our nervous system. The real tragedy isn’t the interaction - it’s that we’ve forgotten how to listen to our bodies. Dextromethorphan in cough syrup? It’s not just a drug. It’s a metaphor. We’re all swallowing numbness and calling it relief.
Betty Kirby
So let me get this straight. You’re telling me that people are dying because they took a cough syrup while on an MAOI? And you’re surprised? Who the hell lets their patients buy OTC meds without checking their med list? This isn’t a medical mystery - it’s incompetence. If your doctor can’t remember your meds, they shouldn’t be allowed to write prescriptions. Period.
Josiah Demara
Buprenorphine is the 'go-to' now? Please. It’s just another opioid with a fancy name. You’re replacing one dependency with another. And don’t get me started on 'non-drug options.' Acupuncture? Heat packs? You’re treating chronic pain like it’s a yoga retreat. This isn’t mindfulness - it’s desperation dressed up as holistic care. Real pain needs real drugs. The problem isn’t the opioids. It’s the fearmongering.
Kaye Alcaraz
Thank you for this vital information. I’m so glad you included the FDA guidelines and the 14-day washout rule. This is exactly the kind of clarity that saves lives. Please keep sharing these resources. We need more awareness, not less. You’ve done a tremendous service to the community.
Erica Banatao Darilag
I’ve been on an MAOI for 8 years. I never knew dextromethorphan was an issue until I read this. I’ve taken Robitussin countless times. I’m going to my pharmacist tomorrow to get a wallet card. Thank you for the warning. I feel less alone now.
Charlotte Dacre
Oh wow. So the solution to opioid-MAOI deaths is... more education? How original. Next you’ll tell us to wash our hands before surgery. Groundbreaking. I’m sure the 11,000 dangerous prescriptions per year are just a coincidence. Maybe if we all just *believe* harder, the deaths will stop. /s
Chiruvella Pardha Krishna
The body is not a machine. It is a symphony. When we interfere with one note - serotonin - we disrupt the entire composition. The opioid is not the enemy. The arrogance of modern medicine is. We think we can control life with pills, when in truth, we are merely guests in the temple of our own biology.
Virginia Kimball
This is why I always tell my friends: if you’re on an MAOI, treat every painkiller like a grenade. I had a friend almost die from tramadol + Nardil. She’s fine now, but she won’t touch anything without checking with her pharmacist first. You’re not being paranoid - you’re being smart. Keep spreading this info. It matters.
Kapil Verma
Americans think they’re entitled to pain relief without consequences. In India, we respect the body’s limits. You think your opioid is safe? You think your cough syrup is harmless? You’re not special. You’re just ignorant. This isn’t about science - it’s about accountability. Stop blaming doctors. Start taking responsibility.
Michael Page
I’ve read this post three times. I’m not sure what to feel. Sad? Angry? Guilty? I’ve prescribed oxycodone to someone on Parnate. I didn’t know. I thought it was 'low risk.' I’m not proud of that. I’m going back to medical school in my head. This isn’t just about drugs. It’s about humility.
Sarah Barrett
The integration of SerotoninSafe into EHRs is a significant step forward. While no system is foolproof, reducing prescribing errors by 76% represents a paradigm shift in patient safety. This is the kind of innovation that transforms reactive medicine into preventive care. Well-documented, well-structured, and critically important.