PML Risk Calculator for Immunosuppressants
Assess Your PML Risk
Progressive Multifocal Leukoencephalopathy (PML) is a rare but serious brain infection caused by the JC virus. This calculator helps you understand your risk based on medication and health factors. Remember: early detection is critical.
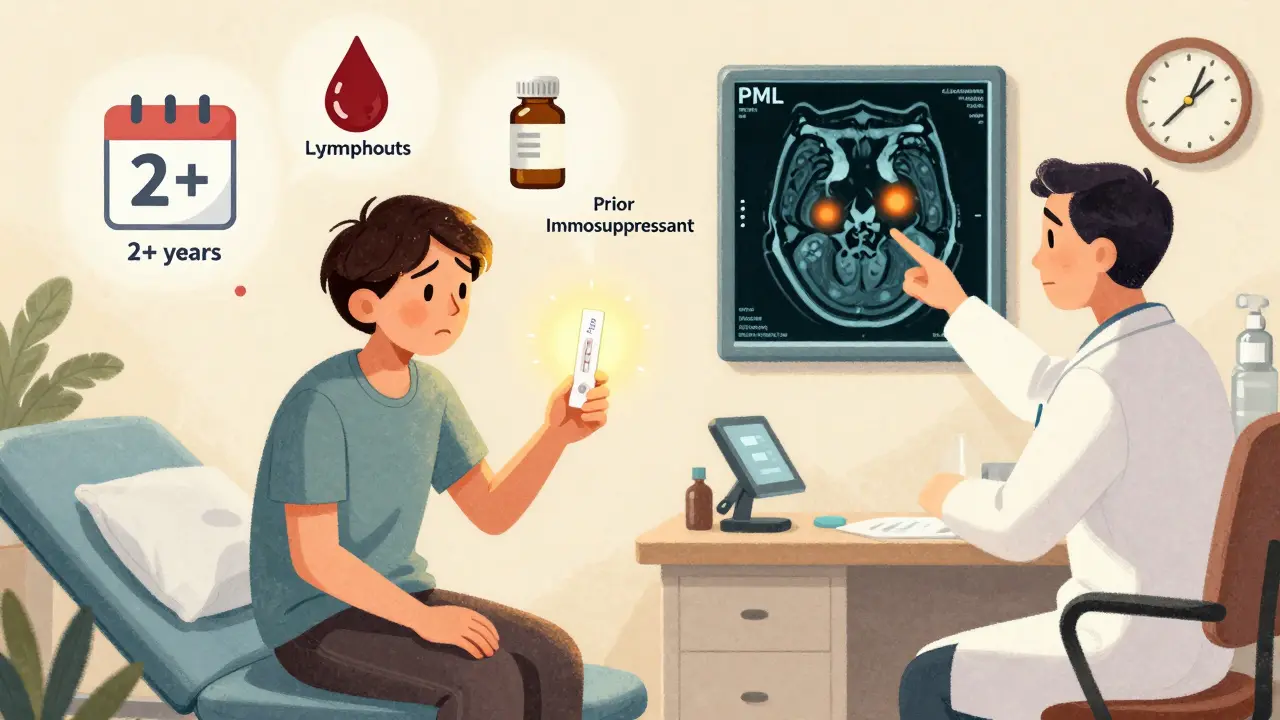
For natalizumab: risk increases after 2 years of treatment.
Counts below 0.8 x 10^9/L increase risk 4.3 times.
Your PML Risk Assessment
Key factors in your calculation:
- Medication: Natalizumab
- JC virus status: Positive
- Prior immunosuppressants: No
- Treatment duration: 1.5 years
- Lymphocyte count: 1.2 x 10^9/L
What Is Progressive Multifocal Leukoencephalopathy (PML)?
PML is a rare but deadly brain infection caused by the John Cunningham (JC) virus. Most people carry this virus without knowing it-between 50% and 70% of adults have been exposed. In healthy people, the immune system keeps it locked down. But when immunity drops, especially from drugs that suppress the immune system, the virus wakes up and starts destroying the protective coating around nerve cells in the brain. This coating, called myelin, is critical for sending signals between brain cells. When it breaks down, the brain can’t communicate properly, leading to worsening neurological problems.
Which Immunosuppressants Carry the Highest Risk?
Not all immunosuppressants are created equal when it comes to PML risk. The drug with the strongest link is natalizumab (brand name Tysabri), used for multiple sclerosis and Crohn’s disease. Through 2011, 102 cases of PML were confirmed in 82,732 patients on natalizumab worldwide-that’s about 0.12% of users. But risk skyrockets in people with three factors: prior use of other immunosuppressants, a positive JC virus antibody test, and treatment lasting longer than two years. In this high-risk group, the rate jumps to 4.1 cases per 1,000 patients.
Other drugs with documented PML cases include:
- Fingolimod (Gilenya): 0.4 cases per 1,000 patient-years
- Dimethyl fumarate (Tecfidera): 0.2 cases per 1,000 patient-years
- Rituximab (Rituxan): 0.8 cases per 1,000 patient-years
- Ibrutinib (Imbruvica): 0.3% incidence in blood cancer patients
Drugs like interferon beta and glatiramer acetate have never been linked to PML in clinical data. That’s why many neurologists now choose these safer options for patients who don’t need aggressive treatment.
How Do Doctors Measure Your Risk?
The biggest tool doctors use is the JC virus antibody test. It checks whether you’ve been exposed to the virus. But it’s not perfect-2% to 3% of people who test negative still carry the virus. That’s why some patients develop PML even with a "negative" result.
For natalizumab users, labs also report an antibody index-a number that shows how strong your immune response to JC virus is. If your index is below 0.9, your risk after four years of treatment is just 0.09%. But if it’s above 1.5, that risk jumps to 10.9%. This number helps doctors decide whether to keep you on the drug or switch.
Another key factor is your lymphocyte count. If your absolute lymphocyte count drops below 0.8 x 10⁹/L, your risk of PML increases 4.3 times. Many doctors now check this blood count every 3 to 6 months, especially if you’ve had other immunosuppressants in the past.
What Are the Early Signs of PML?
PML doesn’t come on suddenly like a stroke. It creeps in slowly. Early symptoms are often mistaken for a multiple sclerosis flare-up. That’s dangerous-delayed diagnosis means worse outcomes. Watch for:
- Mild trouble speaking or slurred speech
- Blurred or lost vision in one eye
- Weakness on one side of the body
- Loss of coordination or clumsiness
- Changes in thinking, memory, or personality
These symptoms don’t always come together. One person might only notice their handwriting getting messy. Another might struggle to find the right words. If you’re on a high-risk drug and notice anything new or different-especially if it lasts more than a few days-tell your neurologist immediately.
Why MRI Scans Are Non-Negotiable
Brain MRIs are the only way to spot PML before it causes major damage. The standard is a scan every 3 to 6 months for patients on natalizumab or other high-risk drugs. But not all MRIs are equal. Special sequences called diffusion-weighted imaging are needed to catch early PML lesions. These look different from regular MS plaques, but it takes training to tell them apart.
Neurologists need 15 to 20 hours of extra training to reliably recognize early PML on MRI. That’s why some community clinics miss it. Academic centers with specialized neuro-radiology teams catch it earlier. If your doctor doesn’t mention regular MRIs, ask why. Waiting until symptoms appear means you’re already in advanced disease.
What Happens After a PML Diagnosis?
Stopping the immunosuppressant is the first step. But that’s not enough. In 50% to 60% of cases, the immune system rebounds too hard, causing something called immune reconstitution inflammatory syndrome (IRIS). This is when your own immune cells attack the brain tissue trying to clear the virus-and that inflammation can be deadly.
Managing IRIS often requires high-dose steroids like methylprednisolone. Some patients recover 90% of function if caught early. Others are left with permanent disability. Mortality remains between 30% and 50%. That’s why early detection saves lives.
What’s Changing in PML Treatment?
There’s new hope. In 2024, a small pilot study of 17 PML patients showed that a new T-cell therapy called DIAVIS cut mortality by 68% and improved movement and speech in most patients. Immune checkpoint inhibitors like pembrolizumab and nivolumab are also being tested-37 cases reported so far, with 27% showing clear improvement.
The Cleveland Clinic is running a Phase II trial (NCT05678901) testing maraviroc, an HIV drug, to prevent PML in high-risk natalizumab users. Early lab data suggests it may block the JC virus from entering brain cells. Results are expected in late 2025.
By 2030, experts predict PML risk with natalizumab could drop to 0.5 cases per 1,000 patient-years thanks to better screening, earlier MRIs, and new treatments. That could make it a viable first-line option again for some patients.
What Patients Are Saying
On patient forums, anxiety about PML is real. In a 2024 survey of 214 people on natalizumab, 78% said they felt "extreme anxiety" about the risk. Sixty-three percent said they’d quit the drug after two years-even if their MS was under control.
One Reddit user, u/MSWarrior2023, shared their story: "After 18 months on Tysabri, my MRI showed early PML lesions. My JC virus test was negative. That 2-3% false negative rate? It’s real."
But there’s also hope. User u/NatalizumabSurvivor wrote: "My neurologist spotted the first lesion on a routine MRI. We stopped Tysabri right away. Six months of steroid treatment for IRIS, and I’ve regained 90% of my motor skills. Early detection saved me."
What You Should Do Now
If you’re on an immunosuppressant:
- Know your JC virus antibody status. Ask for the index number, not just positive/negative.
- Ask if your doctor checks your lymphocyte count every 3 to 6 months.
- Get a brain MRI every 3 to 6 months with diffusion-weighted imaging. Don’t accept a standard MS scan.
- Track any new neurological symptoms-even small ones-and report them immediately.
- Ask about alternatives if you’ve had prior immunosuppressants or have a high JC virus index.
Don’t wait for symptoms. PML doesn’t wait.

12 Comments
Kunal Kaushik
This is some heavy stuff. I’ve been on Tecfidera for 3 years and never thought about PML until now. Glad I’m not one of those high-risk cases. Still, I’ll be asking my neurologist about the JC index next visit. 🙏
Keith Harris
Oh please. They’re scaremongering again. You know what’s *actually* dangerous? Big Pharma pushing drugs they know will kill people and then charging $80k a year. PML? That’s just a side effect they conveniently buried in the 47-page consent form. Wake up, sheep.
Joy Johnston
I’m a nurse in neurology and I see this every day. The key is not avoiding meds-it’s monitoring. JC index + lymphocyte counts + DWI MRIs = your safety trifecta. If your doc isn’t doing all three, find one who does. Seriously. I’ve seen patients lose their lives because they trusted a ‘normal’ MRI.
Joseph Cooksey
You know what’s really terrifying? That this entire conversation hinges on a virus most people carry without ever knowing. We’re all walking time bombs with a 50-70% chance of harboring a silent assassin in our skulls. And the only thing standing between us and brain destruction is a blood test that’s wrong 3% of the time? That’s not medicine. That’s Russian roulette with a neurologist’s pen.
Zachary French
Wait so you’re telling me that some guy in a lab can look at my blood and say ‘yo you got the ghost virus’ and then I’m doomed if I take my MS meds? And they call this science? I’ve seen documentaries where they say the JC virus is just a myth to sell MRIs. Who even made this up? Some pharma bot?
Katherine Urbahn
I must insist: the notion that ‘early detection saves lives’ is not merely a suggestion-it is an imperative. To neglect routine diffusion-weighted imaging is not negligence; it is a breach of the Hippocratic Oath. Patients must be educated, not coddled. The data is unequivocal: delay equals disability.
Amit Jain
Simple truth: if you’re on Tysabri more than 2 years and your JC virus test is positive, switch. No debate. I’ve seen too many people wait for symptoms. By then, it’s too late. Get the index, get the MRI, move on.
Jesse Naidoo
I’ve been on Rituximab for lymphoma. My doc never mentioned PML until I googled it. Now I’m terrified every time I get a headache. Is it normal? Or is my brain turning to mush? Why didn’t anyone tell me this before I started?
Alec Stewart Stewart
Hey, I’m just here to say-you’re not alone. I was scared too. But my doc caught my PML lesion on a routine scan. I didn’t have symptoms. I did the steroids. I’m walking again. It’s scary, but it’s not a death sentence if you’re paying attention. Keep asking questions. 💪
Daz Leonheart
you got this. i know it feels like the world is falling apart when you hear pml, but you’re already ahead of the game just by reading this. stay calm, stay informed, and don’t let fear make your decisions. your doc’s job is to help you-not scare you. we’re rooting for you.
Shelby Price
I’m curious-how common is it for people to get PML from fingolimod if they’ve never taken another immunosuppressant? The article says 0.4 per 1000, but does that include people with prior meds? I’m trying to compare risks.
Caleb Sutton
They’re lying. The JC virus test is a scam. The real cause of PML is 5G towers and the CDC’s secret mind-control program. They use immunosuppressants to mask the symptoms so you don’t notice your brain is being hacked. They’ve been doing this since 2008. Check the FDA’s leaked documents.