When your skin breaks out in scaly patches and your fingers swell like sausages, it’s not just coincidence. These aren’t two separate problems - they’re two signs of the same hidden disease: psoriatic arthritis. It’s an autoimmune condition that attacks both your skin and your joints at the same time, often before you even realize they’re connected. For many, the red, flaky plaques on their elbows or knees come first. But for others, it’s the morning stiffness in their toes or the ache behind their knees that starts it all. Either way, if you have psoriasis and suddenly feel joint pain, you need to pay attention - because this isn’t just aging or overuse. This is psoriatic arthritis.
How Skin and Joints Are Connected
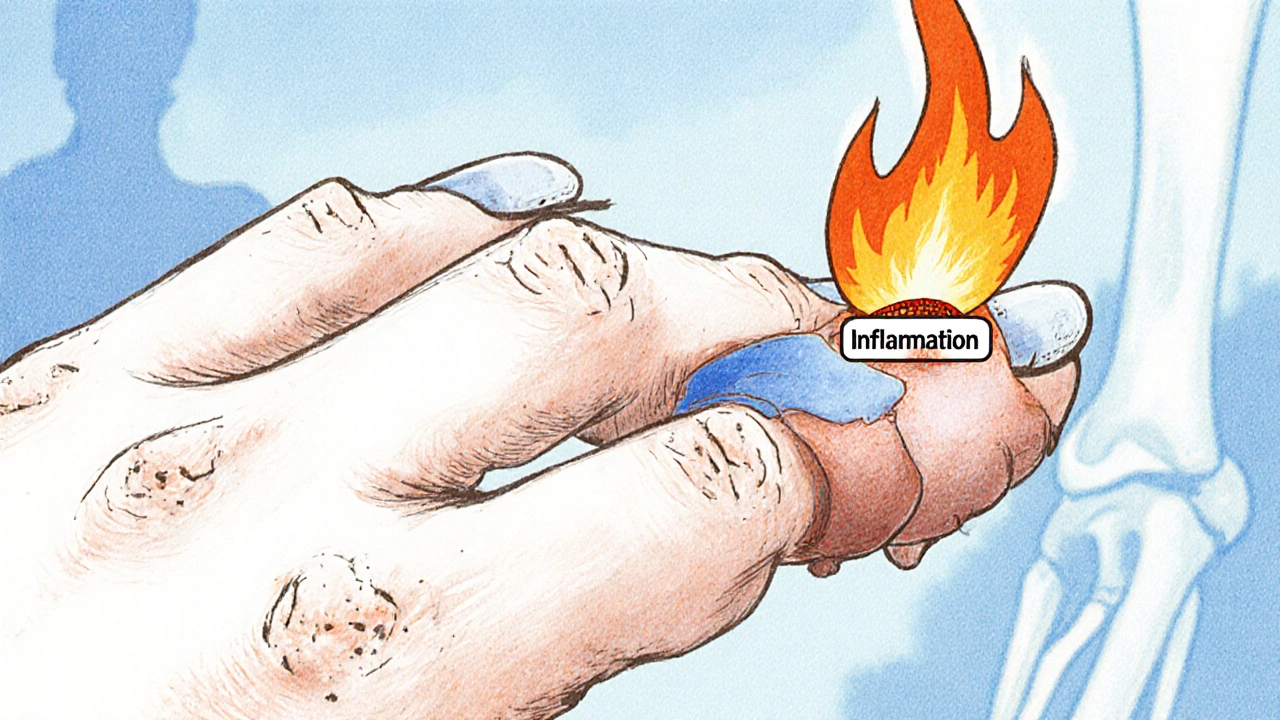
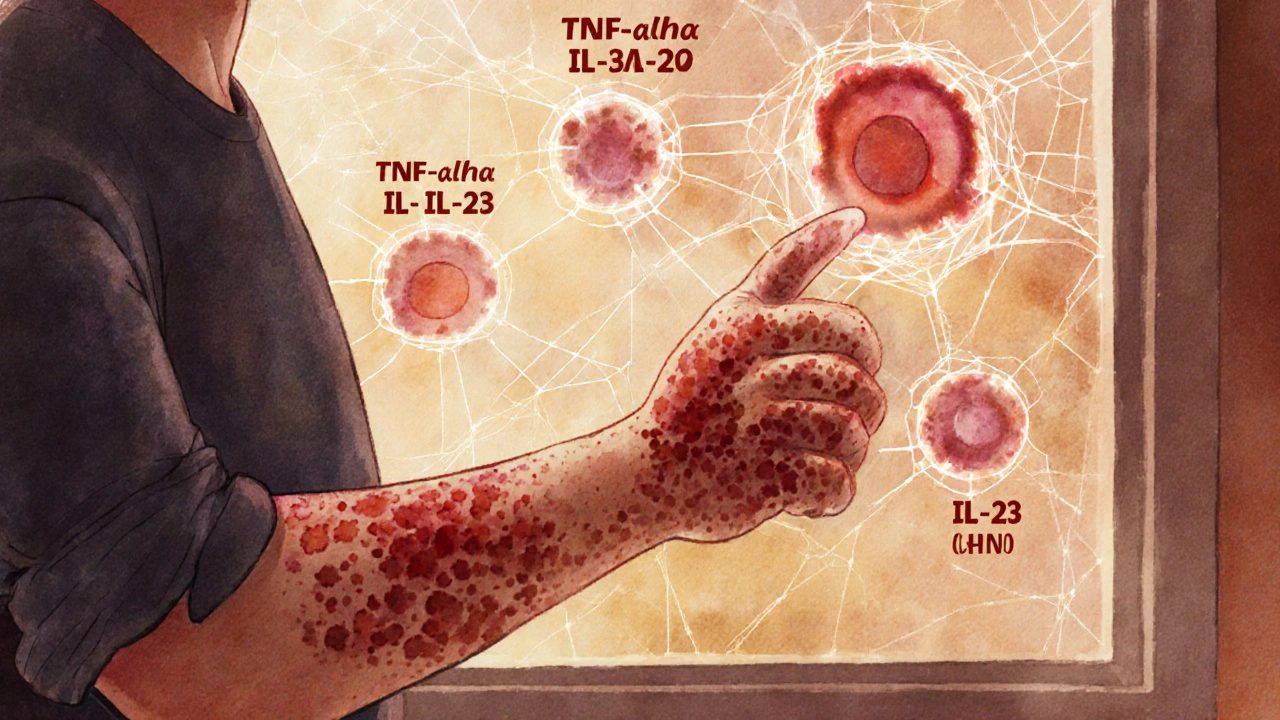
The immune system in psoriatic arthritis doesn’t just get confused - it goes on a double attack. It targets the skin’s outer layer, causing the thick, silvery plaques of plaque psoriasis. At the same time, it inflames the lining of your joints (synovium) and the spots where tendons and ligaments meet bone (entheses). That’s why you can have flaky skin on your scalp and swollen fingers by lunchtime. The same immune signals - TNF-alpha, IL-17, IL-23 - are driving both outbreaks. It’s not random. It’s the same fire burning in two places.
Eighty to ninety percent of people with psoriatic arthritis also have nail changes. Pitting, ridges, or the nail pulling away from the bed (onycholysis) aren’t just cosmetic. They’re red flags. In fact, if you have psoriasis and notice even one of these nail changes, your risk of developing joint pain jumps significantly. The distal joints - the ones closest to your fingernails - are the most commonly affected. That’s unusual. Most types of arthritis start in the knuckles or wrists. Psoriatic arthritis? It often begins right where your nail meets your finger.
Key Signs You Can’t Ignore
There are three classic signs that scream psoriatic arthritis - not just regular arthritis.
- Dactylitis: One or more fingers or toes swell up completely, looking like little sausages. It’s not just puffiness - it’s a deep, uniform swelling that makes the whole digit stiff and tender. About half of all patients experience this.
- Enthesitis: Pain where tendons attach to bone. Think heel pain that feels like you stepped on glass - that’s plantar fasciitis from enthesitis. Or pain behind your knee where the Achilles tendon meets the heel. These aren’t just strains. They’re inflammatory.
- Asymmetric joint pain: If your right knee is swollen but your left knee is fine, and your left wrist is stiff but your right wrist isn’t, that’s a hallmark. Rheumatoid arthritis hits both sides equally. Psoriatic arthritis? It plays favorites.
Some people develop spondylitis - inflammation in the spine - which can cause lower back pain that improves with movement. Others get arthritis mutilans, a rare but severe form that eats away at the bones, causing fingers to shorten or collapse. It’s extreme, but it shows how powerful this disease can be if left unchecked.
Why Diagnosis Takes So Long
The average person waits over two years to get a correct diagnosis. Why? Because doctors often mistake it for rheumatoid arthritis or just “wear and tear.” There’s no single blood test. No antibody like rheumatoid factor that says yes or no. In fact, 90% of people with psoriatic arthritis test negative for it. That leaves doctors relying on signs: the skin, the nails, the pattern of swelling, and imaging.
Ultrasound and MRI can show inflammation in the joints and entheses long before X-rays show damage. But not every clinic has access. And if you’re seeing a dermatologist for your psoriasis, they might not think to check your joints. Meanwhile, your rheumatologist might not know your skin history. That’s why the best outcomes come from teams - dermatologists and rheumatologists working together. About 45% of cases are first spotted by dermatologists. If you’re seeing one, ask: “Could this be psoriatic arthritis?”
Treatment That Actually Works
There’s no cure - but there’s control. And today’s treatments are far more powerful than they were 15 years ago.
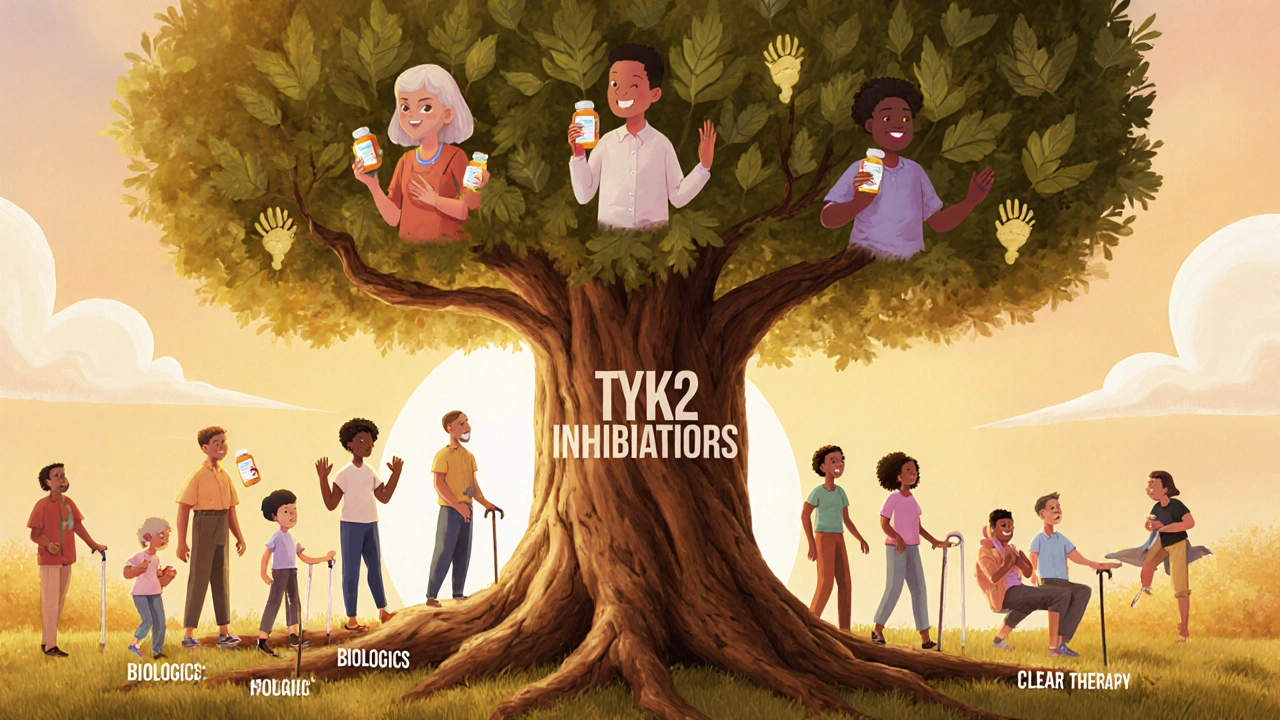
Traditional drugs like methotrexate and sulfasalazine (DMARDs) still help some people, especially in early stages. But for most, biologics are the game-changer. These are targeted injections or infusions that block the specific immune signals causing the damage.
- TNF inhibitors (like adalimumab, etanercept) were the first. They work well for skin and joints, but about 30% of patients don’t respond fully.
- IL-17 inhibitors (secukinumab, ixekizumab) are especially strong for skin, often clearing plaques completely. They also reduce joint swelling.
- IL-23 inhibitors (guselkumab, risankizumab) are newer and show deep, lasting results. One patient reported morning stiffness dropped from two hours to 20 minutes within six weeks.
- TYK2 inhibitors (deucravacitinib) are the first oral option approved specifically for psoriatic arthritis. No needles. Just a daily pill.
What’s surprising? You might need to try more than one. On average, patients go through 2.3 different treatments before finding the right one. That’s frustrating - but it’s normal. The goal isn’t just pain relief. It’s minimal disease activity - meaning no swelling, no new damage, and no fatigue dragging you down.
What Happens If You Wait
Delaying treatment isn’t just about discomfort. It’s about permanent damage. Research shows that 30% of untreated patients develop significant joint destruction within two years. Once bone erodes, it doesn’t grow back. You can’t reverse it. That’s why experts say: treat within 12 weeks of symptoms starting. Do that, and you have a 75% chance of preventing long-term damage.
And it’s not just joints. People with psoriatic arthritis have a 1.5 times higher risk of heart disease. The same inflammation hurting your skin and joints is also damaging blood vessels. That’s why managing this isn’t just about pills - it’s about lifestyle. Quitting smoking, losing weight if needed, and moving daily aren’t optional. They’re part of the treatment plan.
Living With It: Real Challenges
Even with good treatment, life isn’t easy. Sixty-five percent of people report injection site reactions - redness, itching, or pain where the drug goes in. Seventy-eight percent pay over $500 a month out of pocket for biologics. Insurance approvals can take over two weeks. Some people get “brain fog” - mental fatigue that doesn’t go away even when the joints feel better.
Learning your triggers matters. Stress, infections, alcohol, or even certain foods can spark a flare. It takes most people 3 to 6 months to figure out what sets theirs off. Keeping a simple journal - noting what you ate, how much you slept, how stressed you felt - helps. And physical therapy? Essential. Gentle movement keeps joints flexible and reduces stiffness. You don’t need to run a marathon. Walking, swimming, or yoga three times a week makes a difference.
What’s Next
The future is getting brighter. AI tools are now predicting who with psoriasis will develop arthritis - with 87% accuracy - using images of their nails and joints. That means earlier screening. Clinical trials are testing new oral drugs that could replace injections. By 2028, genetic testing may tell you which drug will work best for you - cutting out the trial-and-error.
Right now, the key is action. If you have psoriasis and any joint pain - even mild - get checked. Don’t wait. Don’t assume it’s just aging. Don’t let someone tell you it’s “just stress.” The connection between your skin and your joints is real. And treating it early changes everything.
Can psoriatic arthritis develop without skin psoriasis?
Yes, but it’s rare. About 15% of people develop joint symptoms before any visible skin rash appears. That’s why doctors need to ask about family history - if you have a close relative with psoriasis, your risk goes up even if your skin looks fine. Still, most people eventually develop skin signs within a few years.
Is psoriatic arthritis the same as rheumatoid arthritis?
No. Rheumatoid arthritis usually affects joints symmetrically - both hands, both knees. Psoriatic arthritis is often asymmetric. It also causes dactylitis (sausage fingers), enthesitis (tendon pain), and nail changes - none of which are common in rheumatoid arthritis. Blood tests are different too: rheumatoid factor is usually positive in rheumatoid arthritis but negative in 90% of psoriatic arthritis cases.
Can diet cure psoriatic arthritis?
No diet can cure it. But some people find that reducing sugar, alcohol, and processed foods helps lower inflammation and reduce flares. Omega-3s from fish or supplements may help a little. The biggest dietary win? Losing excess weight. Every pound lost reduces pressure on joints and lowers overall inflammation. It’s not a cure - but it’s a powerful support tool.
Do biologics make you more likely to get infections?
Yes, they suppress part of your immune system, so you’re more vulnerable to infections like colds, flu, or tuberculosis. That’s why everyone starts with TB and hepatitis screening before beginning treatment. You’ll need to avoid live vaccines and report fevers or persistent coughs right away. But for most, the benefits of stopping joint damage far outweigh the risks - especially when monitored closely.
How often do you need to get blood tests while on treatment?
Usually every 3 to 6 months. Your doctor will check liver function, blood cell counts, and kidney health. Some drugs require more frequent monitoring. If you’re on a biologic, you’ll also get screened for TB and hepatitis before starting and occasionally after. It’s not just about safety - it’s about making sure the treatment is working without harming your body.

17 Comments
Pallab Dasgupta
This is the kind of post that makes me want to hug my dermatologist and my rheumatologist at the same time. I had dactylitis for six months before anyone connected it to my scalp psoriasis. They thought I had gout. GOUT. I’m 32. I don’t drink. I don’t eat organ meats. I eat kale like it’s my job. Turns out my immune system just hates me. But now I’m on secukinumab and my fingers don’t look like overcooked hot dogs anymore. Thank you for writing this.
Agastya Shukla
From a clinical perspective, the IL-23/Th17 axis is the central driver here-not just for skin, but for enthesial inflammation too. The fact that TYK2 inhibitors like deucravacitinib target downstream signaling in this pathway is a major leap forward. What’s fascinating is how the same cytokines (IL-23, IL-17) that upregulate keratinocyte hyperproliferation also activate osteoclasts in the joint. It’s not two diseases-it’s one systemic immune dysregulation with phenotypic divergence. The nail changes? They’re not just markers-they’re early biomarkers of entheseal involvement. If you’re seeing pitting, you’re already in the pre-radiographic phase of joint damage.
Emily Craig
So let me get this straight-you’re telling me my 3am finger pain isn’t just because I slept weird? And that my dermatologist wasn’t just being lazy when she didn’t ask about my knees? Wow. I feel like I’ve been gaslit by the entire medical system for the last 4 years. I’m gonna print this out and tape it to my rheumatologist’s forehead.
Josh Zubkoff
Look, I get it. You’re all excited about biologics like they’re magic wands. But have you ever tried getting insurance to approve one? I’ve been on hold for 90 minutes, got denied twice, and my copay is $800 a month. Meanwhile, the pharma reps are out here handing out free samples like candy while the rest of us are selling organs on the dark web. And don’t even get me started on the ‘lifestyle changes’-yeah, I’ll just quit my job, move to a yoga retreat in Bali, and eat only organic kale smoothies. I have a mortgage. I have kids. I have a cat who thinks I’m a vending machine. This isn’t a wellness blog. It’s a survival guide for people who got screwed by their immune system and the healthcare industrial complex.
fiona collins
Ask your dermatologist. That’s it. Just ask. If they don’t know, ask for a referral. You don’t need to be an expert. You just need to be persistent.
Rachel Villegas
I’ve had psoriasis since I was 14. My first joint pain was in my right big toe at 28. I thought it was from wearing tight shoes. Two years later, I got diagnosed. The nail pitting? I thought it was just bad manicures. The heel pain? Plantar fasciitis. The fatigue? Burnout. I didn’t connect the dots until my foot swelled up like a balloon. Now I’m on guselkumab. My skin is clear. My joints don’t scream at 6am. But the emotional toll? That’s still there. It’s not just the pain. It’s the loneliness of being misunderstood.
giselle kate
Who funded this? Big Pharma? They want you to believe you need a $10,000-a-year injection to fix something your body was meant to handle. The real cause? Glyphosate. GMOs. 5G. Your body is detoxing. Your immune system is trying to protect you. They don’t want you to know that. They want you dependent. Try turmeric. Try fasting. Try getting off processed food. Not a single biologic in sight. You’re being sold a lie.
Shivam Goel
Wait, so if you have psoriasis and joint pain, you automatically have PsA? What about reactive arthritis? What about Lyme? What about gout? What about fibromyalgia? You’re oversimplifying a complex differential diagnosis. And you’re ignoring that 15% who get joint symptoms first-how do you rule out RA or spondyloarthropathy without HLA-B27? Or CRP? Or ESR? You can’t just look at nail pitting and call it a day. This is dangerous advice for people who don’t have access to specialists. You’re creating a generation of self-diagnosers who’ll show up at ERs demanding biologics because they read a Reddit post.
Ellen Sales
I’m 52. I’ve had psoriasis for 30 years. I thought my stiff fingers were just getting old. Then I woke up one morning and couldn’t grip my coffee cup. I cried. Not because of the pain. Because I thought I was losing my independence. I went to three doctors before someone listened. Now I’m on a pill. Not a shot. A pill. And I can hold my grandbaby’s hand again. I don’t care what the science says. I care that I can hug her. That’s the cure.
Leisha Haynes
Someone above said they’re on secukinumab and their skin is clear? Cool. But what about the fact that 30% of people still have residual joint pain? And the fatigue? The brain fog? The insurance battles? The fact that you have to carry a letter from your doctor just to get through airport security because you’re on an immunosuppressant? This isn’t a success story. It’s a maintenance nightmare. And no one talks about the grief. The grief for the body you used to have.
Archana Jha
Psoriatic arthritis is just the government’s way of testing how much we’ll tolerate before we wake up. They put the chemicals in the water. The fluoride. The aspartame. The 5G towers. Your skin and joints are screaming because your body knows something’s wrong. The real cure? Detox with bentonite clay and drink lemon water every morning. And stop watching the news. Your stress is making it worse. Also, your dermatologist is probably on the payroll. Ask them about the real cause.
Aki Jones
Let’s be real: the entire psoriatic arthritis narrative is built on flawed biomarkers. TNF-alpha inhibitors? They work for some. But why? Because we don’t understand the heterogeneity of the disease. We’re treating a symptom cluster like it’s a single entity. And the ‘12-week window’? That’s not evidence-based-it’s a marketing slogan from the ACR. And the AI tools predicting onset? Trained on biased datasets. Most studies exclude low-income populations. You think this is science? It’s corporate medicine dressed up in jargon. We need systemic change, not more injections.
Andrew McAfee
As someone from a country where healthcare isn’t a luxury, I’ve seen people with PsA wait years for treatment. In rural India, they use turmeric paste and acupuncture. In Brazil, they use NSAIDs until they can’t walk. The fact that we have biologics at all is a miracle. But the real tragedy? The people who never get diagnosed because they can’t afford to see a dermatologist. This post is brilliant. But it’s for the privileged. We need global access, not just better science.
Amy Hutchinson
Hey I just read this and I have psoriasis and my knee has been hurting for months and I didn’t think it was related but now I’m scared should I go to the doctor right now or wait until Monday? I’m so nervous I’m crying right now
Andrew Camacho
Okay, so here’s the truth no one wants to say: this isn’t about medicine. It’s about control. The system wants you to believe you need lifelong drugs to survive. But what if your body just needed rest? What if your gut was screaming? What if your trauma was manifesting as inflammation? I healed my PsA with fasting, cold plunges, and therapy. No drugs. No needles. Just me, my will, and a damn good therapist. You don’t need a biologic. You need to face your pain. The inflammation? It’s just your soul trying to speak.
Arup Kuri
Everyone’s so obsessed with biologics and doctors but nobody talks about how your mindset shapes your immune system. I had PsA for 5 years. I was angry. I blamed everyone. Then I started meditating. I forgave my dad. I stopped scrolling. I stopped comparing. And guess what? My skin cleared. My joints stopped hurting. It wasn’t the medicine. It was me letting go. You’re not broken. You’re just holding on too tight.
Elise Lakey
I was diagnosed last year. I’m 29. I didn’t know what dactylitis was until I Googled it after my toe swelled up. I felt so alone. Then I found a small online group. We share journal entries. We send each other memes. We remind each other: you’re not your disease. This post? It’s the first time I’ve seen someone explain this without making it sound like a textbook. Thank you. I’m not cured. But I’m not broken either.