Shoulder pain doesn’t just make lifting a coffee mug hard-it can wreck your sleep, ruin your workout, and turn simple tasks like reaching for a shelf into daily battles. If you’ve been told you have rotator cuff issues or bursitis, you’re not alone. Millions of people over 40 deal with this exact problem, and most don’t need surgery. But getting better? That takes knowing exactly what’s going on-and doing the right things at the right time.
What’s Really Going on in Your Shoulder?
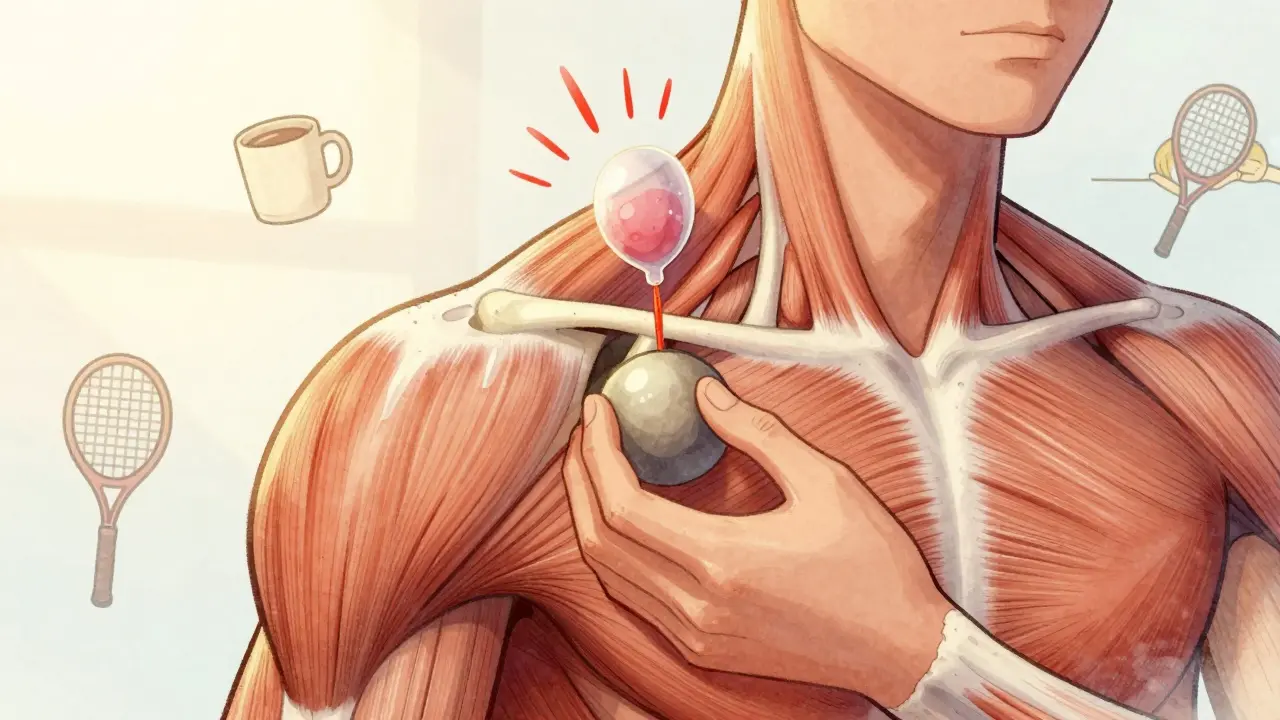
Your shoulder is a ball-and-socket joint, but unlike your hip, it’s built for movement, not stability. That’s where the rotator cuff comes in. It’s not one muscle-it’s four: supraspinatus, infraspinatus, teres minor, and subscapularis. These tiny muscles hold the ball of your arm bone tightly in the socket while you lift, reach, or throw. When they get irritated or worn down, you get rotator cuff tendinitis or even a tear. Right above them sits the subacromial bursa-a fluid-filled sac the size of a walnut that acts like a cushion between the tendons and the bony roof of your shoulder (the acromion). When this bursa swells up from overuse or friction, you’ve got bursitis. The two often happen together because the swollen bursa presses on the tendons, and the inflamed tendons rub harder on the bursa. It’s a vicious cycle. The classic sign? The painful arc. When you raise your arm sideways, it hurts between 60 and 120 degrees-right where the tendons and bursa get pinched. Pain often flares at night, especially if you roll onto that shoulder. It’s not sharp like a cut-it’s a deep, dull ache that lingers.Why Most People Get This After 40
It’s not just aging. It’s repetition. Construction workers, painters, swimmers, tennis players, and even people who type all day with poor posture are at higher risk. Studies show 20-30% of people between 50 and 59 have rotator cuff changes on imaging-even if they don’t feel pain. By 80, that number jumps to over half. The real culprit? Impingement. Over time, the acromion (that bony hook above your shoulder) can develop spurs or change shape. Every time you raise your arm, it grinds against the tendons and bursa. Think of it like a rope fraying against a rough edge. The body tries to heal it, but constant motion keeps the damage going. That’s when inflammation sets in-and pain follows.What Doctors Do First: The Non-Surgical Roadmap
Here’s the truth: 80% of people with rotator cuff tendinitis or bursitis get better without surgery-if they stick to the plan. The first step isn’t a needle or a scalpel. It’s rest, ice, and patience.- Rest: Avoid overhead reaching, lifting heavy things, or sleeping on the sore side for 2-4 weeks. That doesn’t mean complete inactivity-just stop what makes it worse.
- Ice: Apply ice packs for 15-20 minutes, 3-4 times a day, especially after activity. No fancy gadgets needed-just a bag of frozen peas wrapped in a towel.
- NSAIDs: Ibuprofen (400-600 mg three times a day) can help reduce swelling and pain. Don’t take these long-term without checking with your doctor.
Rehab Is the Real Game-Changer
This is where most people fail. They get pain relief from ice or a shot, then go right back to lifting weights or painting ceilings-and the pain comes back. Real recovery starts with rehab. Physical therapy isn’t about massage or heat packs. It’s about rebuilding control. The most effective rehab has three phases:- Range of Motion (Weeks 1-3): Start with pendulum exercises. Lean forward, let your arm hang loose, and gently swing it in small circles. Do this 5-10 minutes, three times a day. It keeps the joint from freezing up without stressing the tendons.
- Scapular Stabilization (Weeks 2-6): Your shoulder blade moves with your arm. If it doesn’t, your rotator cuff has to work harder. Practice squeezing your shoulder blades together like you’re holding a pencil between them. Do 3 sets of 15 reps daily. Patients who do this consistently recover 30% faster than those who don’t.
- Strengthening (Weeks 4-12): Use resistance bands-not weights. Start with light tension (30-50% of your max). Do external rotations (elbow bent at 90 degrees, band anchored to a doorknob, rotate your hand outward) and internal rotations. Do 2 sets of 15 reps, every other day. Progress slowly. Pain should stay below a 5 on a 0-10 scale.

When Surgery Might Actually Help
Surgery isn’t the first choice. In fact, a major 2022 study found no difference in outcomes between patients who had arthroscopic surgery (removing inflamed bursa and shaving down the acromion) and those who did intensive physical therapy alone. Surgery is only recommended if:- You’ve tried 3-6 months of rehab and injections with no improvement
- You have a full-thickness tear (seen on MRI), especially if you’re over 60
- Your job or lifestyle demands full shoulder function (e.g., professional athlete, carpenter)
What Doesn’t Work (And What Could Hurt You)
Avoid these common traps:- Waiting too long to start rehab: The longer you stay inactive, the more your shoulder stiffens. Early movement is key.
- Doing too much too soon: Pushing through sharp pain or doing heavy lifting before your tendons are ready? That’s how you turn a tear into a bigger tear.
- Skipping scapular work: Focusing only on the rotator cuff is like fixing a car’s tires but ignoring the suspension. Your shoulder blade controls the whole system.
- Overusing steroid shots: More than 2-3 a year increases tendon rupture risk by 8%.
Real People, Real Results
A 54-year-old carpenter from Ohio stopped working for 12 weeks, did daily pendulum exercises and scapular squeezes, and returned to full duty without surgery. A 37-year-old tennis player used eccentric strengthening (slowly lowering a band against resistance) and cryotherapy after every session-and was back in tournaments in 10 weeks. But here’s the flip side: 35% of people who return to sports too early end up back in the clinic. Weekend warriors who play golf or lift weights on Saturday after a week of desk work? That’s a recipe for repeat injury.
What’s New in 2026
The field is moving fast. In 2024, the FDA approved a new ultrasound-guided injection system that improves accuracy from 72% to 94%. That means fewer misplaced shots and less risk. Platelet-rich plasma (PRP) injections are now a second-line option after steroids fail. Studies show a 68% success rate for PRP versus 52% for repeat steroid shots. For older adults, blood flow restriction training-using a cuff to limit blood flow during light exercise-is showing promise. It builds strength faster without heavy loads, cutting recovery time by 30% for people over 60. And wearable sensors? Companies are developing devices that clip onto your shirt and give real-time feedback on your shoulder form during rehab exercises. Imagine getting a gentle buzz on your arm if you’re shrugging instead of scapular retracting.How to Stay on Track
The biggest reason rehab fails? Inconsistency. Most people think they’re doing enough. They’re not.- Use a phone app with reminders. Patients who did this completed 82% of their exercises. Those who didn’t? Only 54%.
- Track your pain daily. Keep a simple log: “Day 12: Pain level 3 during band rotations, no pain at night.”
- Find a therapist who gives you video demos. 63% of patients who got video instructions said they stuck with rehab longer.
When to See a Doctor
Go in if:- Pain lasts more than 2 weeks despite rest and ice
- You can’t lift your arm above shoulder height
- You feel weakness when trying to hold something
- Pain wakes you up at night
- You had a fall or sudden pop in your shoulder
Can rotator cuff pain go away without surgery?
Yes-about 80% of cases improve with non-surgical treatment. Rest, ice, physical therapy, and sometimes a steroid injection are enough. Surgery is only considered after 3-6 months of consistent rehab with no progress.
How long does shoulder bursitis take to heal?
Most people start feeling better in 2-4 weeks with rest and ice. Full recovery, including strength and movement, takes 8-12 weeks with consistent rehab. Rushing back to activity too soon can cause setbacks.
Is it safe to exercise with shoulder bursitis?
Yes-but only the right exercises. Avoid overhead lifting, pushing, or pulling. Focus on gentle range-of-motion moves like pendulums and scapular squeezes. Pain should stay mild (under 5/10). If it spikes, stop and rest.
What’s the best sleeping position for shoulder pain?
Sleep on your back with a pillow under the affected arm, or on the opposite side with a pillow hugged to your chest. Avoid sleeping on the sore shoulder. Some people find relief using a wedge pillow to keep the shoulder elevated slightly.
Can I use heat for shoulder bursitis?
Avoid heat in the first 48-72 hours after pain starts-it can increase swelling. After that, gentle heat before stretching can help loosen stiffness, but ice is still better for active pain or after exercise.
How many physical therapy sessions do I need?
Most people need 2-3 sessions per week for the first 4 weeks, then 1-2 sessions per week for another 4-8 weeks. Daily home exercises (20-30 minutes) are just as important as the clinic visits.
Will corticosteroid injections cure my shoulder pain?
No-they reduce inflammation and give you a window of relief so you can do rehab more effectively. They don’t fix the underlying problem. Relying on them without physical therapy leads to recurrence. Limit them to 2-3 per year.
Can I prevent rotator cuff pain from coming back?
Yes. Keep doing your scapular stabilization exercises 2-3 times a week even after you feel better. Maintain good posture, avoid prolonged overhead work, and warm up before any activity that involves your shoulders. Prevention is easier than recovery.

13 Comments
Linda O'neil
Just finished my 8-week rehab program and I can finally reach the top shelf again. No surgery, no magic pills-just pendulum swings and scapular squeezes every damn day. It’s boring as hell but it works. Trust the process.
Also, sleeping on your back with a pillow under your arm? Game changer. I used to wake up screaming.
jonathan soba
Interesting how you casually mention that 80% don’t need surgery without acknowledging that most of those people are middle-class Americans with access to PT and time off work. In the UK, if you’re not rich, you wait 18 months for a referral and then get told to ‘take ibuprofen and live with it.’ This reads like an ad for physical therapy clinics.
matthew martin
Man, I used to think shoulder pain was just ‘getting old.’ Then I started doing those dumb little pendulum things like a zombie and-boom-three months later I’m back lifting weights without wincing. Who knew the secret sauce wasn’t some fancy machine or steroid shot but just… moving your shoulder blade like you’re trying to hold a pencil between your shoulder blades?
It’s like your body’s got a secret language and the rotator cuff is just whispering, ‘Hey, don’t forget about me.’
Also, PRP injections? Sounds like a vampire’s smoothie but apparently it’s real. Wild times.
Chris Urdilas
So let me get this straight-you’re telling me the solution to chronic shoulder pain is… doing the exact same boring exercises every day for months? No wonder people give up. I tried this for two weeks, got bored, went back to lifting, and now I’ve got a tear that’s basically a tiny rope fraying in a hurricane.
But hey, at least I didn’t waste money on a $200 resistance band. I just used my old yoga strap. Efficiency.
Jeffrey Carroll
This is an exceptionally well-structured and evidence-based overview of non-surgical management of shoulder pathology. The emphasis on scapular stabilization as a foundational component of rehabilitation is clinically sound and aligns with current biomechanical research. I would recommend this resource to all patients presenting with subacromial impingement syndrome.
Phil Davis
They say ‘rest and ice’ like it’s some mystical cure. I rested. I iced. I cried into my frozen peas. Still couldn’t reach my own damn back. Then I found out my posture was so bad my spine looked like a question mark. Turns out, your shoulder doesn’t care how much you lift-it cares if your rib cage is even vaguely aligned.
So now I sit like a statue. And I hate it. But my shoulder doesn’t hate me anymore.
Irebami Soyinka
USA thinks it’s the only country that has shoulder pain? LOL. In Nigeria, we don’t have PT clinics-we have uncles who rub coconut oil and say ‘God will heal you.’ But guess what? Some of them still carry 50kg sacks on their heads at 70 and don’t even flinch. You people overthink everything. Just move your arm. Stop reading blogs.
😂💪🏽
doug b
Do the exercises. Every day. Even if you’re tired. Even if you’re sore. Even if you think you’re doing it wrong. You’re not. Your body remembers what it needs. I coached my dad through this-he was 68, never exercised, now he’s playing golf again. No magic. Just consistency.
And if you’re not doing scapular squeezes? You’re wasting your time. That’s the real MVP.
Mel MJPS
I’ve been dealing with this for two years. I thought I was just lazy. Turns out I just didn’t know how to move right. The pendulum exercise felt so silly I did it in my kitchen while making coffee. Now I can reach for my coffee cup without wincing. Thank you for making this feel less scary.
Jess Bevis
PRP works. Tried it. Still did PT. No magic, just better timing.
Rose Palmer
It is imperative to emphasize that adherence to the prescribed rehabilitation protocol is the single most predictive factor for successful non-operative outcomes. The data presented in this article is methodologically robust and reflects current clinical best practices. I would encourage all patients to engage with licensed physical therapists to ensure proper exercise execution and progression.
Mindee Coulter
Scapular squeezes are the real MVP. I did them while watching Netflix. No one knows. I’m a genius.
Timothy Davis
Let’s be real-this article cherry-picks the best-case scenarios. 80% improve? Sure, if you’re young, healthy, have insurance, and don’t have a job that requires you to lift 40-pound boxes all day. What about the 20% who get worse? Or the ones who get steroid shots and then rupture their tendon because they were told to ‘just keep moving’? This reads like a PR piece from a rehab chain. No one talks about the real cost-time, money, lost income. This isn’t advice. It’s a fantasy.