Metronidazole Alternatives – Your Quick Guide
When you need Metronidazole alternatives, drugs that can replace metronidazole for bacterial or protozoal infections, often offering different dosing or side‑effect profiles, they become a crucial part of everyday prescribing. Also known as metronidazole substitutes, these options let doctors avoid intolerance, drug interactions, or resistance issues tied to the original medication. One of the most common swaps is Tinidazole, a long‑acting nitroimidazole that works similarly but requires fewer doses, making it popular for treating trichomoniasis and giardiasis. Another frequently mentioned choice is Clindamycin, a lincosamide antibiotic effective against anaerobic bacteria when metronidazole can’t be used. By comparing these agents, clinicians can match the right drug to the right patient while keeping therapy simple and safe. Metronidazole alternatives therefore aren’t just backup pills; they’re tailored solutions that address specific infection types, patient allergies, and dosing convenience.
Understanding the Class and the Resistance Challenge
The core of this discussion lies in the Nitroimidazole class, a group of drugs that includes metronidazole, tinidazole, and ornidazole, all targeting anaerobic microbes and certain protozoa. While the class is effective, growing antibiotic resistance, the ability of bacteria to survive drug exposure, pushes doctors to consider alternatives earlier in treatment. The relationship can be expressed as: the Nitroimidazole class influences resistance patterns, and resistance patterns, in turn, shape the selection of metronidazole alternatives. For example, in regions with high metronidazole‑resistant Helicobacter pylori, tinidazole often outperforms the original drug because of its slightly different pharmacokinetics. Meanwhile, clindamycin steps in when anaerobic infections arise in patients who cannot tolerate nitroimidazoles due to nausea or neuropathy. By recognizing how resistance drives drug choice, prescribers can avoid trial‑and‑error cycles and move straight to the most likely effective agent.
Choosing the right substitute hinges on three practical factors: the infection site, patient tolerance, and dosing schedule. For pelvic inflammatory disease or bacterial vaginosis, tinidazole’s single‑dose regimen can improve adherence compared with a three‑day metronidazole course. In surgical prophylaxis where a broad anaerobic coverage is needed, clindamycin’s IV formulation offers rapid serum levels and penetrates tissue well. Additionally, special populations—pregnant women, the elderly, or those with liver impairment—often benefit from alternatives with fewer systemic side effects. The semantic connection here is clear: Metronidazole alternatives require an assessment of infection type, patient health, and safety profile to guide optimal selection. Below you’ll find a curated list of articles that dive deeper into each option, compare their efficacy, and provide real‑world tips for safe prescribing. Explore the collection to see how these alternatives stack up in different clinical scenarios and get actionable insights you can apply today.
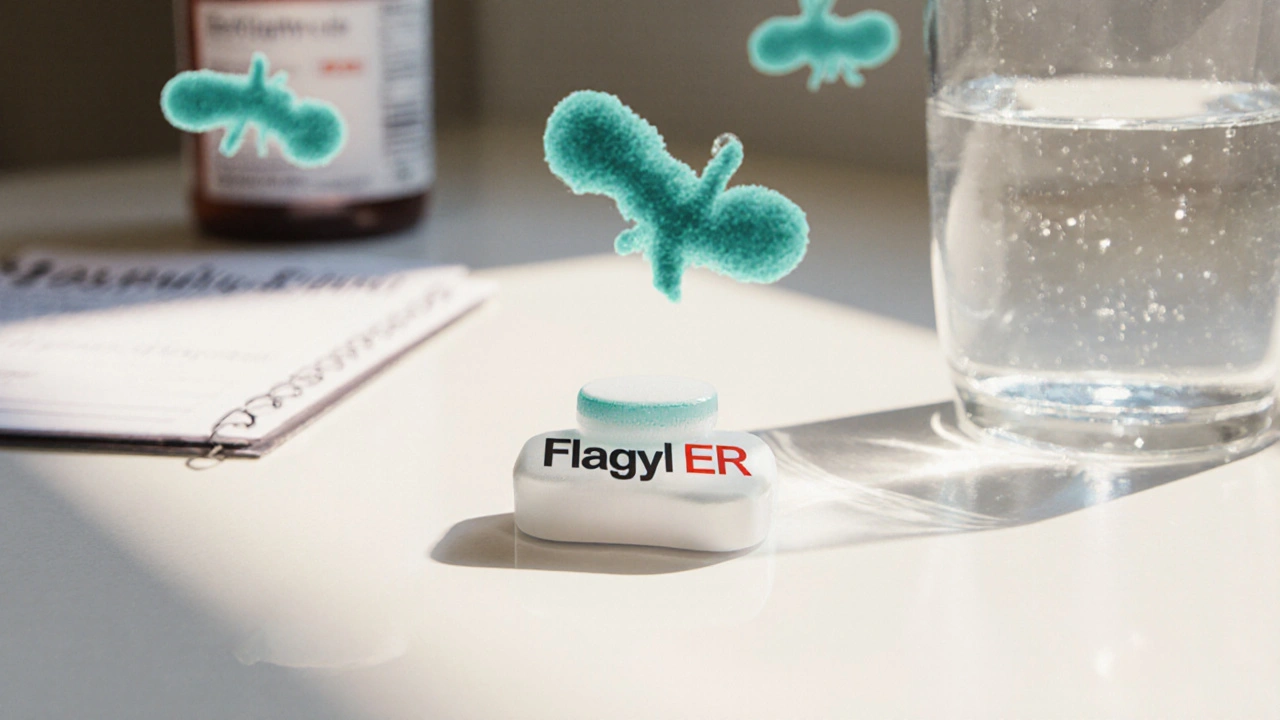
Flagyl ER vs Alternatives: Metronidazole Comparison Guide
- Beata Staszkow
- |
- |
- 20
A practical guide comparing Flagyl ER (Metronidazole) with key alternatives, covering efficacy, side effects, cost, and best-use scenarios.
View more