Introduction: The Growing Importance of Pulmonary Embolism Treatments
As a blogger who has been closely following the latest advances in research and medicine, I am thrilled to share with you the future of pulmonary embolism treatment. This life-threatening condition has affected many individuals, but recent breakthroughs are paving the way for better outcomes and improved quality of life. In this article, we will explore the latest advances in pulmonary embolism research, novel treatment options, and what the future holds for patients suffering from this condition.
Understanding Pulmonary Embolism: Causes and Symptoms
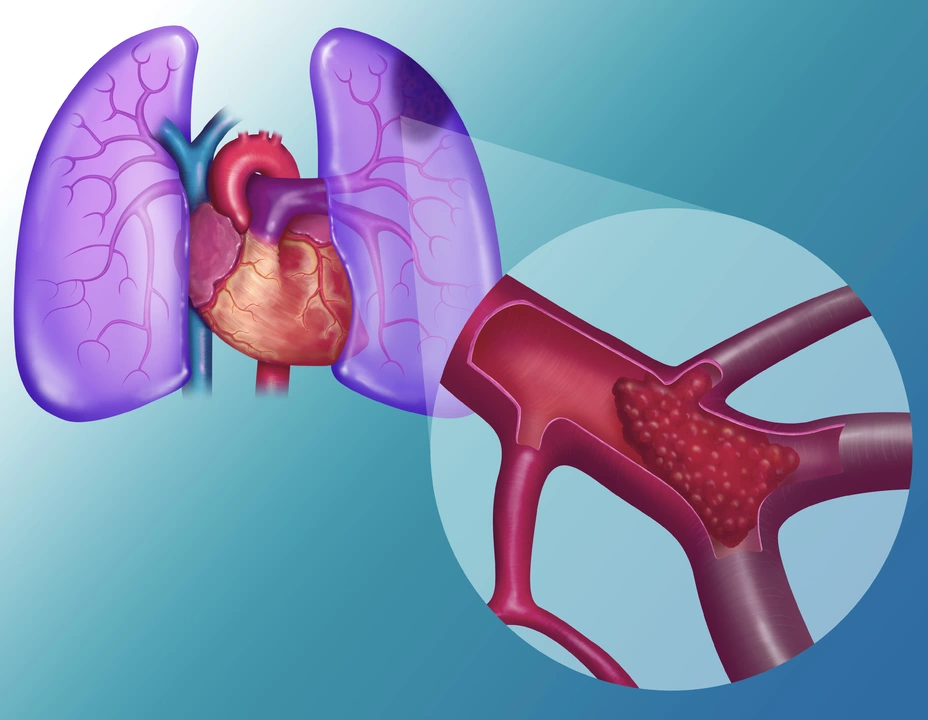
Before diving into the future of pulmonary embolism treatment, let's first understand what this condition entails. A pulmonary embolism occurs when a blood clot, usually from the legs or pelvis, travels to the lungs and blocks a blood vessel. This can lead to potentially life-threatening complications, such as low blood oxygen levels, lung damage, and even heart failure. Common symptoms include shortness of breath, chest pain, and coughing up blood. Identifying and treating pulmonary embolism early is crucial for better patient outcomes.
Current Treatment Options: Anticoagulants and Thrombolytics
Currently, the primary treatment for pulmonary embolism involves the use of anticoagulants, or blood thinners, which help prevent new clots from forming and existing clots from growing. Thrombolytics, or clot-dissolving medications, are also sometimes used in more severe cases. While these treatments have proven effective, they do come with potential side effects, such as increased bleeding risks. This has prompted researchers to explore alternative, more targeted treatment options to improve patient outcomes.
The Role of Catheter-Directed Therapy
One promising development in pulmonary embolism treatment is catheter-directed therapy (CDT). This minimally invasive procedure involves inserting a catheter through a vein in the groin or neck and guiding it to the site of the clot in the lungs. Once in position, the catheter is used to deliver targeted medications or mechanical devices to break up or remove the clot. CDT has shown promise in reducing the risk of bleeding complications and improving patient outcomes, particularly in those with severe pulmonary embolism.
Exploring New Medications: Finding the Right Balance
As researchers continue to investigate new medications for the treatment of pulmonary embolism, finding the right balance between efficacy and safety remains a priority. Recent advances have led to the development of novel oral anticoagulants, which offer more convenient dosing regimens and fewer drug interactions than traditional options. Additionally, ongoing clinical trials are exploring the potential of targeted thrombolytics, which could offer a more precise approach to clot dissolution while minimizing the risk of bleeding complications.
The Promise of Personalized Medicine
Personalized medicine is poised to play a significant role in the future of pulmonary embolism treatment. By tailoring treatment strategies to individual patients based on factors such as genetic makeup, lifestyle, and medical history, healthcare providers can potentially improve treatment effectiveness while minimizing side effects. As our understanding of the genetic and molecular underpinnings of pulmonary embolism continues to grow, the potential for personalized medicine in this field becomes increasingly promising.
Prevention Strategies: Reducing the Risk of Pulmonary Embolism
While advances in treatment options are essential, reducing the risk of pulmonary embolism through preventive measures remains a critical component of patient care. Strategies such as regular exercise, maintaining a healthy weight, and avoiding prolonged periods of immobility can help reduce the risk of blood clot formation. Additionally, healthcare providers can play a key role in identifying patients at high risk for pulmonary embolism and implementing appropriate preventive measures, such as the use of compression stockings or prophylactic anticoagulation therapy.
Technological Innovations: Improving Diagnosis and Treatment
As technology continues to advance, its role in the diagnosis and treatment of pulmonary embolism is likely to expand. From sophisticated imaging techniques to innovative medical devices, these technological innovations have the potential to improve patient outcomes and streamline the care process. For example, artificial intelligence algorithms are being developed to assist in the accurate and timely diagnosis of pulmonary embolism, while advances in bioengineering are paving the way for the development of novel clot-removal devices.
Conclusion: A Bright Future for Pulmonary Embolism Treatment
As we look to the future of pulmonary embolism treatment, it's clear that advances in research and medicine are driving significant progress in this field. From novel medications and personalized treatment strategies to innovative technologies, the future holds immense promise for patients suffering from this life-threatening condition. As a blogger passionate about health and medical innovation, I am excited to continue following these developments and sharing them with you, as we strive for a world where pulmonary embolism is effectively managed and treated for all.

15 Comments
Vanessa Guimarães
Oh, wonderful, another glossy piece about cutting‑edge pulmonary embolism cures that will apparently solve everything overnight. Let's not forget that every "breakthrough" is just another way for Big Pharma to line its pockets while pretending to care about our health. If you think the future is bright, perhaps you've been living under a rock where the only air is filtered through a corporate press release.
Lee Llewellyn
Well, here we go again with the endless parade of so‑called medical miracles that supposedly will turn pulmonary embolism into a footnote of history. First, you have the antiquated anticoagulants, which have been around since the dawn of modern medicine and, surprise surprise, still cause bleeding complications that make every patient fear their own prescription. Then, the eager hype machines tout catheter‑directed therapy as though a tiny tube magic wand can replace decades of clinical expertise, ignoring the fact that these procedures require highly specialized skill sets and expensive equipment that most community hospitals simply cannot afford. Moreover, the touted novel oral anticoagulants, while convenient, have introduced a whole new set of drug‑drug interactions that can be a nightmare for the poly‑pharmacy patient already juggling hypertension, diabetes, and cholesterol meds. Let’s not forget the dazzling AI algorithms that claim to diagnose pulmonary embolism with uncanny accuracy; while impressive on paper, they rely on massive data sets that are often riddled with bias, potentially leading to misdiagnosis in minority populations. In addition, the personalized medicine paradigm, though theoretically promising, is still stuck in the lab with genetic panels that are costly, time‑consuming, and, frankly, not yet validated for routine clinical use. The prevention strategies mentioned-exercise, weight management, compression stockings-are fine, but they gloss over the socioeconomic reality that many at‑risk patients cannot afford gym memberships or even proper nutrition. And while we cheer for technological innovations, the reality is that the rollout of these advanced devices will be uneven, leaving rural and underserved communities behind. All this glitters in your article, but beneath the surface lies a litany of logistical, financial, and ethical challenges that no one seems willing to address honestly. So, before we celebrate the "bright future," let’s keep our boots firmly on the ground and demand real, equitable solutions that consider the everyday patient, not just the idealized research cohort.
Drew Chislett
Great rundown! The shift toward catheter‑directed therapies and AI‑assisted diagnostics really feels like a hopeful step forward. It's encouraging to see researchers tackling both efficacy and safety, especially with the newer oral anticoagulants that simplify dosing. I’m optimistic that these advances will make a tangible difference for patients who previously faced daunting treatment choices.
Rosalee Lance
Indeed, the march toward personalized medicine invites us to contemplate the very nature of health and autonomy. If we can align treatment with an individual's genetic fingerprint, we begin to honor the philosophical principle that each life is a unique tapestry, not a generic template. Yet, the specter of surveillance looms-who holds the data, and how might it be wielded? In a world where information is power, we must guard against an unseen oligarchy shaping our very biology.
Nonetheless, the promise remains: a future where interventions are as precise as a poet's meter, delivering relief without the collateral damage of blanket therapies.
Kara Lippa
Well‑written summary; I appreciate the clear explanation.
Puneet Kumar
From an inclusive perspective, the integration of advanced catheter‑directed interventions into standard protocols can serve as a catalyst for capacity building across diverse health systems. By fostering cross‑border knowledge exchange, we enrich the global lexicon of pulmonary embolism management while simultaneously addressing disparities in access to high‑tech solutions. Moreover, employing precise terminology-such as "mechanical thrombectomy" versus the colloquial "clot‑busting"-ensures that interdisciplinary teams communicate efficiently, reducing procedural errors and optimizing patient outcomes.
michael maynard
Look, I get the whole mentorship vibe, but honestly, the hype around these gadgets feels like a corporate PR stunt. You keep talking about "capacity building" while ignoring the fact that most hospitals can't even afford a decent scanner, let alone a fancy catheter system. It’s like bragging about a brand‑new sports car when you live in a city with no roads.
Roger Bernat Escolà
Another day, another miracle cure promise-because what we really need is drama, not data. These new therapies sound like a Hollywood script, but the reality for patients is still fear, uncertainty, and long recovery times. If only the medical community could focus less on spectacle and more on solid outcomes.
Allison Metzner
It's fascinating how the narrative shifts from rigorous science to theatrical hype, almost as if the stakes are being raised for the sake of audience applause.
william smith
The key takeaway is that early diagnosis combined with appropriate anticoagulation remains the cornerstone of treatment, and emerging technologies should be viewed as adjuncts rather than replacements.
Timothy Javins
While that sounds reasonable, I can’t help but wonder whether these “adjuncts” might actually complicate the clinical picture and increase costs without clear benefit.
Kay Yang
Really appreciate the balanced view here 😊 It’s good to see both optimism and caution presented in the same piece.
Rajesh Kumar Batham
Absolutely! The blend of new tech and tried‑and‑true methods feels like the best path forward 🙌
Bill Gallagher
In reviewing the recent literature on pulmonary embolism therapeutics, one must first acknowledge the historical reliance on vitamin K antagonists-a paradigm that, while effective in certain cohorts, was irrevocably limited by its pharmacokinetic variability, dietary interactions, and the necessity for routine INR monitoring; subsequently, the advent of direct oral anticoagulants (DOACs) introduced a paradigm shift predicated upon predictable pharmacodynamics, reduced monitoring burden, and favourable safety profiles, albeit at the expense of higher acquisition costs, limited reversal agents, and occasional concerns regarding off‑label use in specific patient subpopulations such as those with severe renal impairment or extreme body mass indexes; furthermore, the integration of catheter‑directed thrombectomy and ultrasound‑assisted thrombolysis represents a nuanced evolution, wherein the mechanical removal of thrombus is complemented by targeted pharmacologic lysis, thereby potentially mitigating systemic hemorrhagic risk-a concept substantiated by emerging data yet constrained by operator expertise, procedural heterogeneity, and the absence of large‑scale randomized controlled trials; it is also imperative to consider the role of artificial intelligence in augmenting diagnostic accuracy through computed tomography pulmonary angiography (CTPA) analysis, a development that promises earlier detection but simultaneously raises questions regarding algorithmic bias, data privacy, and the interpretive training required for clinicians; finally, the pursuit of personalized medicine, through genomic profiling and biomarker identification, holds prospective promise for stratifying patients according to thrombotic propensity and therapeutic responsiveness, though the translational gap from bench to bedside remains substantial, necessitating robust clinical validation, cost‑effectiveness analyses, and equitable access to ensure that the envisioned future does not exacerbate existing health disparities.
Rajashree Varma
What a thorough synthesis; it’s uplifting to see the field moving toward both precision and compassion. Let’s keep the momentum while ensuring every patient benefits.