Understanding Prilocaine and Its Use in Medicine
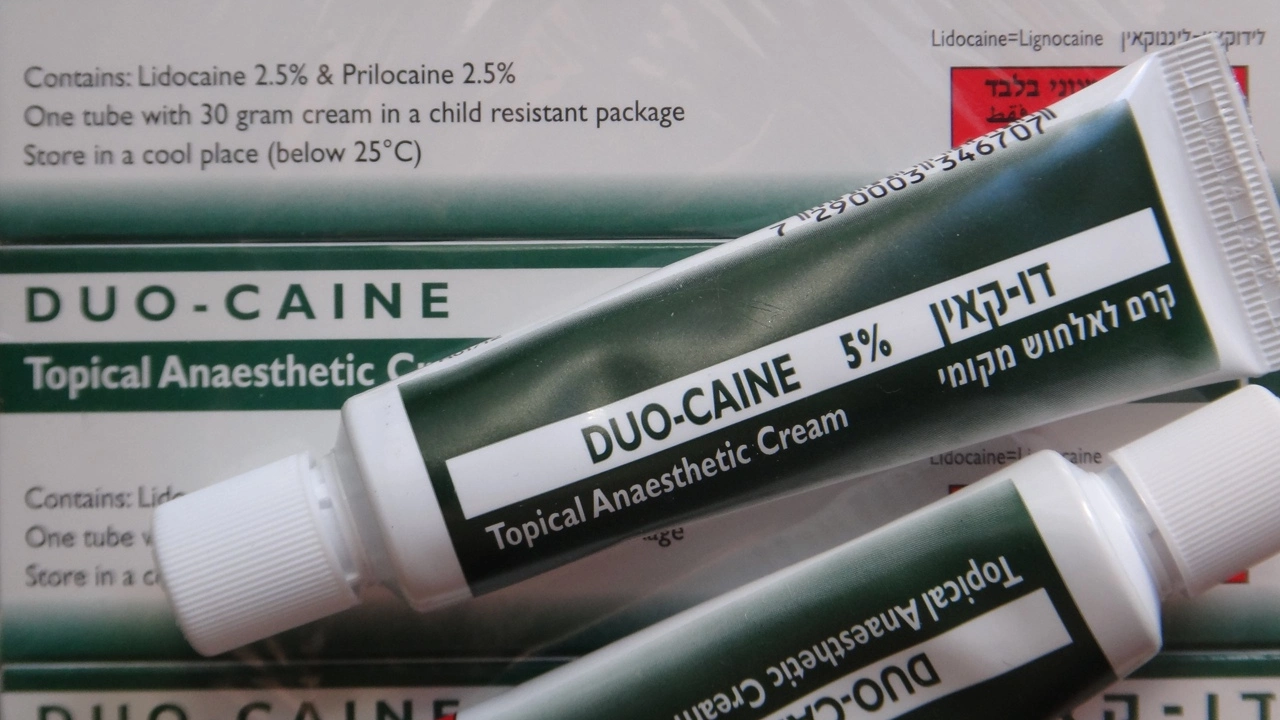
Before diving into the specific use of prilocaine in ophthalmic surgery, it's necessary to have a basic understanding of what prilocaine is and its general use in the field of medicine. Prilocaine is a type of local anesthetic commonly used in various medical and dental procedures. It works by blocking nerve signals in your body, thereby reducing pain or discomfort. One of the key benefits of prilocaine is that it has a rapid onset of action and a moderate duration of effect, making it an ideal choice for many types of procedures.
The Importance of Anesthesia in Ophthalmic Surgery
Eye surgeries, like all other surgical procedures, require the use of anesthesia. Anesthesia is a vital part of ophthalmic surgery as it helps to numb the eye, making the procedure painless for the patient. It also helps to relax the muscles around the eye, making it easier for the surgeon to perform the operation. The type of anesthesia used can greatly affect the outcome of the surgery, hence the reason why prilocaine is often the go-to choice for many ophthalmic surgeons.
Prilocaine in Ophthalmic Surgery: A Closer Look
Prilocaine has been found to be very effective in ophthalmic surgeries. Its rapid onset and moderate duration of effect make it an ideal anesthetic for procedures that do not require a long duration of anesthesia. Moreover, prilocaine has a lower risk of causing systemic toxicity compared to other local anesthetics, which is another reason why it is often preferred in ophthalmic surgery.
Comparing Prilocaine with Other Local Anesthetics
When compared to other local anesthetics, prilocaine stands out for several reasons. Firstly, it has a faster onset of action. This means that it starts working quicker, numbing the area faster than other anesthetics. Secondly, it has a moderate duration of effect. This means that it lasts just long enough for most ophthalmic procedures to be completed. Lastly, prilocaine has a lower risk of systemic toxicity, making it a safer choice for patients.
Side Effects and Risks Associated with Prilocaine
Like all medications, prilocaine does come with potential side effects and risks. Some common side effects include minor skin irritation at the site of injection, slight dizziness, and occasional headaches. More serious but rare side effects can include severe allergic reactions, slow heart rate, and low blood pressure. Despite these potential side effects, the benefits of prilocaine in ophthalmic surgery often outweigh the risks, especially when administered by a skilled and experienced ophthalmic surgeon.
Post-Operative Care After Prilocaine Use
After undergoing ophthalmic surgery with prilocaine, it's important to follow certain post-operative care instructions to ensure a smooth and speedy recovery. This includes avoiding touching or rubbing the eye, keeping the eye clean, and using prescribed eye drops as instructed. Any side effects or discomfort experienced after the surgery should be reported to the ophthalmologist immediately.
Conclusion: The Integral Role of Prilocaine in Ophthalmic Surgery
Prilocaine has proven to be a valuable tool in the armamentarium of ophthalmic surgery. Its rapid onset of action, moderate duration of effect, and lower risk of systemic toxicity make it an ideal choice for many eye surgeries. Despite potential side effects, when administered correctly, prilocaine can greatly enhance the comfort and safety of patients undergoing ophthalmic surgery.

10 Comments
mausumi priyadarshini
While prilocaine is praised for its rapid onset, its lower toxicity claim is overstated, and alternatives deserve equal consideration.
Taryn Bader
Prilocaine seems like the star of the show, but honestly, it’s just another local anesthetic. The quick kick‑in is nice, yet the duration can leave you hanging if the surgery drags. I’m not saying it’s bad, just that the hype feels a bit overblown. Folks should weigh it against lidocaine or bupivacaine before jumping in.
Myra Aguirre
Fair point, the quick onset can be handy, and the duration does vary with the procedure.
Shawn Towner
One could argue that the emphasis on toxicity is a red herring; the real issue lies in pharmacokinetic variability among patients, which isn’t addressed by simple “lower risk” statements.
Ujjwal prakash
When we look at the dosage guidelines, prilocaine is typically administered at 1‑2 mg/kg for ocular blocks, which translates to about 0.5 ml of a 4% solution per injection site. The concentration allows for a swift onset, usually within 2‑3 minutes, and the anesthetic effect lasts roughly 30‑45 minutes-enough for most cataract or pterygium excisions. Moreover, its vasoconstrictive properties reduce systemic absorption, mitigating the risk of methemoglobinemia that we sometimes see with higher concentrations of other agents. However, practitioners must monitor for signs of cardiac depression, especially in patients with pre‑existing heart conditions, because even the “moderate” systemic toxicity can become significant at the upper end of the dosing range.
In practice, combining prilocaine with a small amount of epinephrine can further prolong the block and improve hemostasis, but this also adds a layer of complexity that requires careful titration.
Diane Helene Lalande
That’s a solid rundown; the dosage specifics and the epinephrine combo are especially useful. Just a tiny note: “vasoconstrictive” might be a mouthful for some readers-maybe a brief definition could help.
Edwin Levita
Honestly, reading about prilocaine feels like watching a low‑budget thriller-lots of hype, but the climax never quite lands. The rapid onset is decent, yet the whole “safe and sound” narrative seems a bit staged.
Xander Laframboise
Let’s dissect the drama surrounding prilocaine point by point. First, the claim of rapid onset is not unique; lidocaine achieves a similar timeline when buffered correctly. Second, the moderate duration is often cited, but in reality, the variability can span from 20 minutes to over an hour depending on tissue vascularity. Third, the alleged lower systemic toxicity is a nuanced statement-while methemoglobinemia incidence is lower than with benzocaine, high doses can still precipitate it. Fourth, the pharmacodynamics differ across ethnicities, with some studies indicating slower clearance in certain populations, which the literature rarely highlights. Fifth, the combination with epinephrine, although extending the block, introduces a risk of ischemic complications in the ocular tissues, especially in patients with glaucoma. Sixth, the technique of injection matters immensely; a misplaced sub‑tenon injection can cause globe perforation irrespective of the anesthetic used. Seventh, postoperative pain profiles are not dramatically improved with prilocaine versus alternatives, suggesting that patient comfort may depend more on surgical technique than on the anesthetic choice. Eighth, cost considerations are often overlooked; prilocaine can be more expensive than generic lidocaine in many markets, affecting accessibility. Ninth, the training curricula for ophthalmology residents frequently emphasize lidocaine, leaving prilocaine as a secondary option, which may reflect institutional bias rather than evidence. Tenth, the regulatory approvals vary by country, with some regions restricting its ophthalmic use due to limited clinical trial data. Eleventh, the literature on long‑term ocular outcomes after prilocaine use is sparse, making it hard to assess any subtle toxic effects on the retina or optic nerve. Twelfth, patient-reported outcome measures rarely differentiate between anesthetics, focusing instead on overall surgical satisfaction. Thirteenth, the risk of allergic reactions, though low, is not negligible, especially in patients with a history of local anesthetic hypersensitivity. Fourteenth, the convenience of a single‑dose vial can be offset by the need for precise dosing calculations in pediatric cases. Finally, while prilocaine certainly has its place, the narrative that it is the superior choice in ophthalmic surgery should be tempered with a critical appraisal of the existing data and an awareness of its limitations.
Jason Petersen
Prilocaine works okay but the data isn’t huge it’s fine for short procedures
Melissa Gerard
Sure, “it’s fine” is the vibe, but honestly it feels like a lazy excuse to skip proper evaluation 🙄.