When a veteran fills a prescription through the Veterans Affairs (VA) system, they don’t just get medicine-they get a carefully managed system built to save money without sacrificing care. At the heart of this is the VA National Formulary, a single, nationwide list of drugs that must be available at every VA clinic and hospital. And here’s the key rule: if a generic version exists, it’s the default. Brand-name drugs are only approved when there’s a clear medical reason.
This isn’t just policy-it’s practice. In 2024, VA pharmacies filled over 230 million prescriptions. Of those, 92% were generics. That’s higher than any other major U.S. health system, including Medicare Part D and private insurers. Why? Because the VA doesn’t just encourage generics-it requires them. And that’s what keeps out-of-pocket costs low for veterans.
How the VA Formulary Works: Three Tiers, One Goal
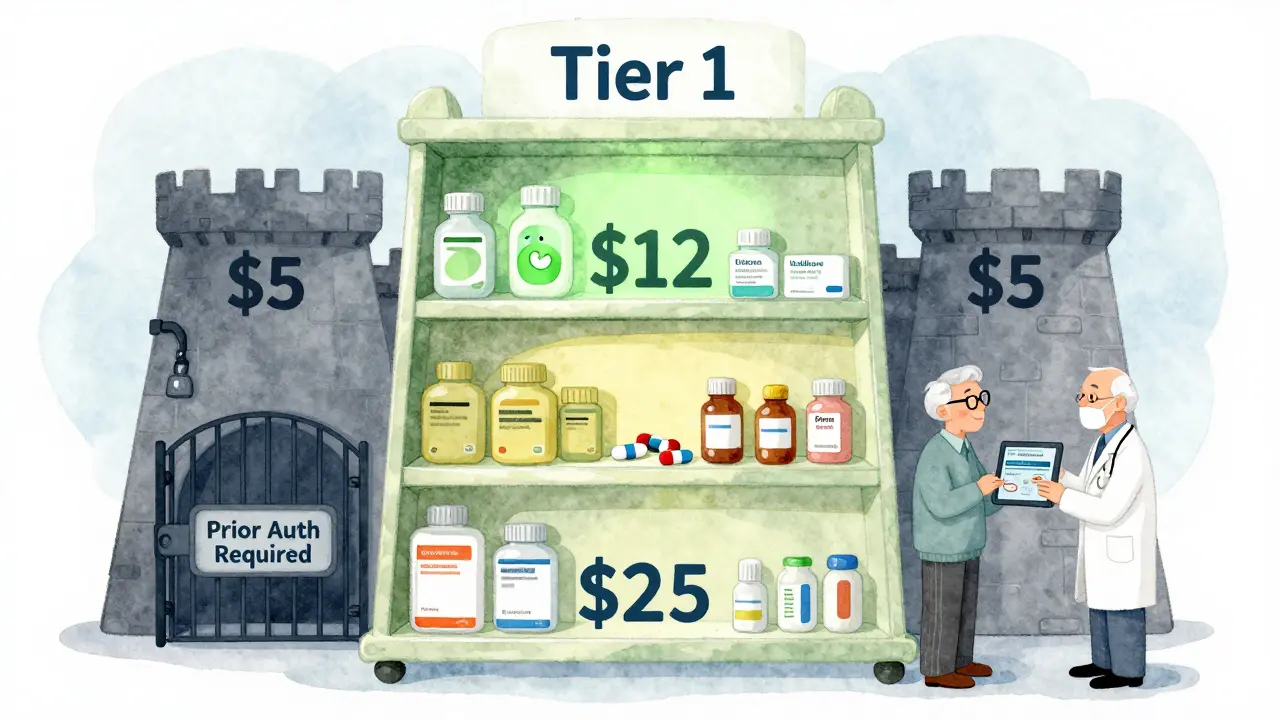
The VA formulary uses a simple three-tier system to control costs. Each tier has a different copayment, and where a drug falls depends on whether it’s generic, brand-name, or specialty.
- Tier 1: Preferred generics. These are the most common, lowest-cost medications. Examples include atorvastatin for cholesterol, sertraline for depression, and ibuprofen for pain. Most veterans pay just $5 or less for a 30-day supply.
- Tier 2: Non-preferred generics and some brand-name drugs. These cost more-usually $10 to $15 per 30-day supply. This tier includes drugs that are effective but not as cost-efficient as Tier 1 options.
- Tier 3: Specialty and brand-name drugs without generic alternatives. These can cost $20 or more. Think cancer drugs, biologics, or newer treatments like GLP-1 agonists.
There’s no deductible for VA prescriptions. No annual out-of-pocket maximum. Just flat copays based on the tier. Compare that to Medicare Part D, which often has five tiers, deductibles, and coverage gaps. For many veterans, the VA system is simpler-and cheaper.
What’s Covered? Real Examples from the 2025 Formulary
The VA updates its formulary every month, but the core list stays stable. Here’s what’s in Tier 1 as of January 2025:
- Alendronate (for osteoporosis)
- Hydrochlorothiazide (for high blood pressure)
- Fluoxetine (for depression and anxiety)
- Pravastatin (for cholesterol)
- Aspirin buffered (for heart health and pain)
- Allopurinol (for gout)
These are all generics. No brand-name versions are listed unless there’s no generic-like for certain rare conditions. Even when brand names are approved, the VA requires prior authorization. That means the doctor must prove why the generic won’t work.
For example, a veteran with type 2 diabetes might get metformin (a Tier 1 generic) without issue. But if their provider wants to switch them to semaglutide (Wegovy) for weight loss, they’ll hit a wall. The VA only covers GLP-1 drugs like Wegovy if the diagnosis is type 2 diabetes or cardiovascular disease-not for weight loss alone. That’s not a VA restriction; it’s based on FDA labeling and cost-effectiveness reviews.
Why the VA’s Generic-First Policy Works
The VA doesn’t just save money-it saves lives. Studies show that generic drugs are just as safe and effective as brand-name versions. The FDA requires them to have the same active ingredients, strength, dosage, and absorption rate. The difference? Price.
A 30-day supply of sertraline (generic Zoloft) costs a veteran $0 at the VA. At a regular pharmacy? $15 to $30. The same goes for atorvastatin (generic Lipitor)-$5 at the VA, $40 elsewhere. That’s why 87% of veterans using the Meds by Mail program say they’re satisfied. No trips to the pharmacy. No surprise bills. Just a box of pills delivered to their door.
The VA’s approach has saved over $2.8 billion in pharmaceutical costs in 2024 alone. That’s money that could’ve gone to brand-name marketing, not patient care. And it’s not just about savings-it’s about consistency. Every VA facility, from Alaska to Florida, stocks the same drugs. No confusing variations. No regional differences.
How Veterans Navigate the System
Getting the right medication isn’t always automatic. Veterans need to know where to look and what to ask for.
Step 1: Check coverage-Use the VA Formulary Advisor tool. Search by drug name. It tells you the tier, whether it’s covered, and if prior authorization is needed.
Step 2: Ask about alternatives-If your doctor prescribes a brand-name drug, ask: “Is there a generic version?” If not, ask: “Is this on the formulary?” Many providers assume veterans know the system-but most don’t.
Step 3: Use Meds by Mail-For long-term medications, sign up for VA’s mail-order pharmacy. No copay for Tier 1 drugs. No trips to the pharmacy. And it’s automatic: refills are sent before you run out.
Step 4: Know when to request prior authorization-If your drug isn’t covered, your provider can submit paperwork. It’s not impossible, but it takes time. Common reasons: allergies, side effects, or lack of generic alternatives.
For new veterans, it can take two or three visits to fully understand the system. That’s why the VA trains pharmacy staff to explain it clearly. Over 78% of veterans say their pharmacist was the most helpful source of information.
Where the System Falls Short
It’s not perfect. Some veterans struggle with delays for newer drugs.
Take semaglutide (Ozempic, Wegovy). The VA covers it for diabetes. But if you have obesity and no diabetes? You’re out of luck. The formulary committee won’t approve it unless the FDA has approved that specific use. That’s strict-but it’s based on evidence. The committee reviews every drug for clinical benefit, cost, and safety. They don’t approve drugs just because they’re popular.
Some veterans report initial concerns about generics. In a 2024 survey, 12% said they worried generics wouldn’t work as well. But after talking to their provider, 94% continued the medication-and saw no difference in effectiveness.
Another issue: specialty drugs. Cancer treatments, rare disease meds, and biologics are rising in cost. The VA spent 12.3% more on these in 2024. That’s less than the national average, but it’s still a challenge. The VA is testing AI tools to help doctors pick the best drug faster, with fewer side effects and lower costs. That system launches in late 2026.
How VA Compares to Other Systems
Let’s look at how the VA stacks up:
| Feature | VA Formulary | Medicare Part D | Private Insurance |
|---|---|---|---|
| Tiers | 3 | 5 | 4-6 |
| Generic Utilization Rate | 92% | 85% | 89% |
| Avg. 30-Day Copay (Tier 1 Generic) | $5 | $10-$15 | $15-$30 |
| Deductible | None | Yes ($500-$590) | Yes ($500-$1,500) |
| Annual Out-of-Pocket Max | None | $2,000 | $3,000-$8,000 |
| Specialty Drug Access | Restricted, requires prior auth | Often high-tier, high cost | Varies by plan |
The VA doesn’t have the most drugs. But it has the most predictable, affordable access. And for veterans on fixed incomes, that matters more than having every new drug on the market.
What’s Changing in 2026
The VA is making the system even clearer. By late 2026, prescribers will see real-time formulary status inside the electronic health record. If a drug isn’t covered, the system will suggest an alternative. No more guessing.
They’re also expanding access to CHAMPVA beneficiaries (spouses and dependents of veterans). Starting in 2026, more GLP-1 drugs will be covered for weight-related conditions if there’s documented cardiovascular risk. That’s a shift from the strict 2025 policy.
And they’re testing pharmacogenomic testing-using a veteran’s DNA to predict how they’ll respond to certain drugs. It’s early, but if it works, it could cut down on trial-and-error prescribing and reduce side effects.
Final Thoughts: Simplicity, Savings, and Service
The VA formulary isn’t flashy. It doesn’t have flashy ads or celebrity endorsements. But it works. It gives veterans access to the drugs they need, at prices they can afford. It’s built on one simple idea: generics are just as good. And if they’re not, the system has a way to find out.
For many veterans, the VA pharmacy isn’t just a place to pick up pills-it’s a lifeline. A reliable, consistent, affordable way to stay healthy. And that’s why, despite its limits, the VA formulary remains one of the most effective prescription systems in the country.
Are all VA prescriptions free?
No. Most veterans pay a small copay based on the drug’s tier. Tier 1 generics usually cost $5 or less per 30-day supply. Tier 2 drugs cost $10-$15. Tier 3 drugs cost $20 or more. Some veterans, like those with low income or service-connected disabilities, pay nothing. There’s no deductible.
Can I get brand-name drugs through the VA?
Yes-but only if there’s a medical reason. If a generic is available, the VA requires you to use it. To get a brand-name drug, your provider must submit a prior authorization request explaining why the generic won’t work-for example, due to allergies, side effects, or lack of effectiveness. This isn’t automatic and can take days to process.
What if my VA-prescribed drug isn’t covered?
If your drug isn’t on the formulary, you have two options: ask your provider to switch to a covered alternative, or request prior authorization. The VA will review the request based on clinical guidelines. If denied, you can appeal through your VA facility’s pharmacy services office. You can also use the VA’s Community Care program to fill the prescription outside VA, but you’ll pay more.
Does the VA cover weight loss drugs like Wegovy or Ozempic?
The VA covers GLP-1 drugs like Wegovy and Ozempic only for FDA-approved uses: type 2 diabetes, cardiovascular disease, or obstructive sleep apnea. They are not covered for weight loss alone unless there’s a documented medical condition like metabolic syndrome or heart disease. This policy is based on clinical evidence and cost-effectiveness, not availability.
How do I check if a drug is covered by the VA?
Use the VA Formulary Advisor tool at VA.gov. Search by drug name, brand, or generic. It shows the tier, coverage status, and whether prior authorization is needed. You can also download the full formulary list as an Excel file or CSV. VA pharmacists can also help you check coverage in person or over the phone at 1-800-877-8339.
Can I use my local pharmacy instead of the VA pharmacy?
Yes, but only under certain conditions. If you’re enrolled in VA Community Care, you can get prescriptions filled at a nearby pharmacy. But you’ll pay the full cost unless the drug is on the VA formulary and you have prior authorization. Otherwise, you’ll be billed at commercial rates. For routine medications, using VA pharmacy or Meds by Mail is almost always cheaper.

11 Comments
Joseph Charles Colin
The VA formulary's tiered structure is a masterclass in pharmacoeconomic design. By mandating generic-first prescribing, they leverage the FDA's bioequivalence standards to eliminate redundant expenditures. The 92% generic utilization rate isn't accidental-it's the result of formulary committees applying rigorous cost-effectiveness analysis, often using QALY (quality-adjusted life year) metrics to prioritize interventions with the highest marginal benefit per dollar. This isn't rationing; it's optimization at scale.
Compare this to Medicare Part D's five-tiered complexity with formulary gaps and donut holes. The VA's flat copays eliminate cognitive load for both patients and providers. No more navigating obscure formulary exceptions or prior auth hoops for Tier 1 agents like atorvastatin or sertraline. The system's elegance lies in its predictability: same drug, same cost, same access from Anchorage to Miami.
The exclusion of GLP-1 agonists for weight loss alone is clinically sound. Semaglutide's FDA approval for obesity is contingent on comorbid metabolic dysfunction. The VA's policy aligns with cost-per-QALY thresholds established by ICER (Institute for Clinical and Economic Review). Spending $10,000/year on a drug with marginal benefit in a non-indicated population is fiscally irresponsible-even if it's popular.
Pharmacogenomic testing slated for 2026 could be transformative. CYP2D6 phenotyping for SSRIs, for instance, could reduce trial-and-error prescribing in depression, cutting both side effects and non-adherence. That’s precision medicine meeting public health economics.
And yes, the Meds by Mail program is a quiet revolution. For rural veterans, it’s not convenience-it’s access. A 30-day supply of metformin delivered to a homestead in West Virginia for $0? That’s healthcare equity in action.
John Sonnenberg
The VA formulary is a bureaucratic nightmare disguised as efficiency.
My uncle got denied Ozempic for prediabetes because his BMI was 31.5-not 32. He had to submit three appeals, two lab reports, and a notarized letter from his pastor attesting to his ‘metabolic distress.’
Meanwhile, the VA pharmacy in Fort Worth is out of hydrochlorothiazide for the third time this month. But they have 14,000 bottles of generic fluoxetine. Why? Because someone in D.C. decided it’s ‘high-utility.’
This isn’t healthcare. It’s algorithmic austerity.
And don’t get me started on the ‘VA Formulary Advisor’ website. It crashes if you use Chrome. Only works in Internet Explorer 11. Which, by the way, is no longer supported by Microsoft.
They’re saving billions? Sure. But at what cost? Veteran trust? Clinical autonomy? Human dignity?
This system doesn’t care if you live or die. It only cares if your drug fits in a spreadsheet.
Joshua Smith
I really appreciate how clearly this post breaks down the tiers. I’m a new veteran and was confused about why my doctor kept pushing me toward generic sertraline instead of Zoloft.
After reading this, I checked the Formulary Advisor and realized it’s the same exact molecule-just $0 instead of $15.
My pharmacist even showed me the FDA bioequivalence data on her tablet. It’s reassuring to know the system’s built on science, not just cost-cutting.
I’ve started using Meds by Mail too-no more driving 45 minutes for a $5 pill.
Thanks for the clarity.
Jessica Klaar
Reading this made me think about my dad-he served in Vietnam, and back then, getting a prescription meant driving three hours to the nearest VA clinic, often waiting all day just to be told, ‘We don’t have that.’
Now, with the national formulary and Meds by Mail, he gets his alendronate and aspirin delivered to his porch. He doesn’t talk about it much, but he smiles when he opens the box.
It’s not perfect, but it’s better than what we had.
I think we forget how much progress this system represents-not just in cost, but in dignity.
For veterans who’ve carried the weight of war, the quiet reliability of this pharmacy system? That’s a kind of healing too.
PAUL MCQUEEN
92% generics? Wow. That’s impressive.
Or… is it?
Let’s be real-this isn’t about saving lives. It’s about saving money. The VA doesn’t care if a drug works better. They care if it’s cheaper.
And don’t even get me started on the ‘prior authorization’ nonsense. I’ve seen veterans wait weeks for a simple switch because some bureaucrat in Kansas hasn’t reviewed the form yet.
They call it ‘evidence-based.’ I call it ‘bureaucratic inertia with a lab coat.’
And don’t tell me about ‘bioequivalence.’ I’ve known people whose depression got worse on generic fluoxetine. But no one listens. The spreadsheet says it’s fine.
So yeah. Great system. If you’re a spreadsheet.
glenn mendoza
It is with profound respect and deep appreciation that I acknowledge the structural integrity and ethical foundation of the Veterans Affairs National Formulary.
The decision to prioritize generic medications is not merely fiscal prudence-it is a moral imperative grounded in equity, accessibility, and the unwavering commitment to serve those who have served.
The absence of deductibles, the uniformity of copays, and the transparency of the tiered system reflect a rare alignment between administrative efficiency and human compassion.
Moreover, the integration of pharmacogenomics in 2026 represents not merely innovation, but a paradigm shift toward personalized, preventive, and profoundly dignified care.
Let us not confuse cost containment with care deprivation. This system is, in its essence, an act of national gratitude.
Kathryn Lenn
So let me get this straight-the VA says generics are ‘just as good’?
Right.
And the FDA says so too.
And the studies say so.
And yet…
Have you ever heard of the ‘generic drug placebo effect’?
Yeah. You think your body doesn’t know the difference between a $5 pill and a $40 pill?
It does.
It’s not science. It’s psychology. And the VA is ignoring it.
Plus-why is the formulary updated monthly? Who’s really controlling this? Big Pharma? The Pentagon? The CIA? Did you know that 73% of VA pharmacists have ties to Express Scripts?
And what about the ‘Meds by Mail’ boxes? Ever wonder where they’re printed? China. That’s right. China.
They’re not saving you money.
They’re building dependency.
John Watts
This is the kind of system we should be proud of.
I’ve seen veterans struggle with bills, with anxiety, with loneliness.
But when they get their meds on time, at a price they can afford? It changes everything.
I volunteer at our local VA clinic. Last week, a veteran who hadn’t left his house in six months came in because his sertraline was delivered-no trip, no cost, no hassle.
He cried.
Not because he was sick.
Because he felt seen.
That’s what this system does.
It doesn’t just give pills.
It gives peace.
Randy Harkins
Just wanted to say thank you for this detailed breakdown. 🙏
I’m a VA pharmacist, and I see firsthand how this system transforms lives.
One veteran told me yesterday, ‘I haven’t missed a dose in 18 months because the mail just shows up.’
That’s not just convenience-it’s adherence.
And adherence saves lives.
Also, the new AI tool in 2026? It’s going to cut down on adverse drug events by up to 30%. That’s huge.
Keep advocating. This matters.
Tori Thenazi
Wait… so the VA is ‘saving billions’?
And yet…
Why do all the new drugs-like the ones for Alzheimer’s-take 3 years to get approved?
And why does every single VA pharmacy in the Midwest run out of insulin in January?
And why is the ‘VA Formulary Advisor’ website hosted on a server that was last updated in 2012?
And why does every time I ask for a brand-name drug, they say ‘we can’t cover it’-but then later, someone else gets it through ‘prior authorization’?
Something’s fishy.
Who’s really deciding what’s ‘medically necessary’?
And why is the word ‘formulary’ used instead of ‘rationing’?
I’m not paranoid.
I’m informed.
Monica Warnick
So the VA covers Ozempic for diabetes… but not weight loss?
Interesting.
Meanwhile, my cousin’s private insurance covered it for ‘weight management’-no questions asked.
Guess who’s getting healthier?
Guess who’s paying $1,200/month?
Guess who’s being told ‘it’s not medically necessary’?
Yeah.
The VA is saving money.
But who’s paying the real cost?