Denosumab: What It Is, How It Works, and What You Need to Know
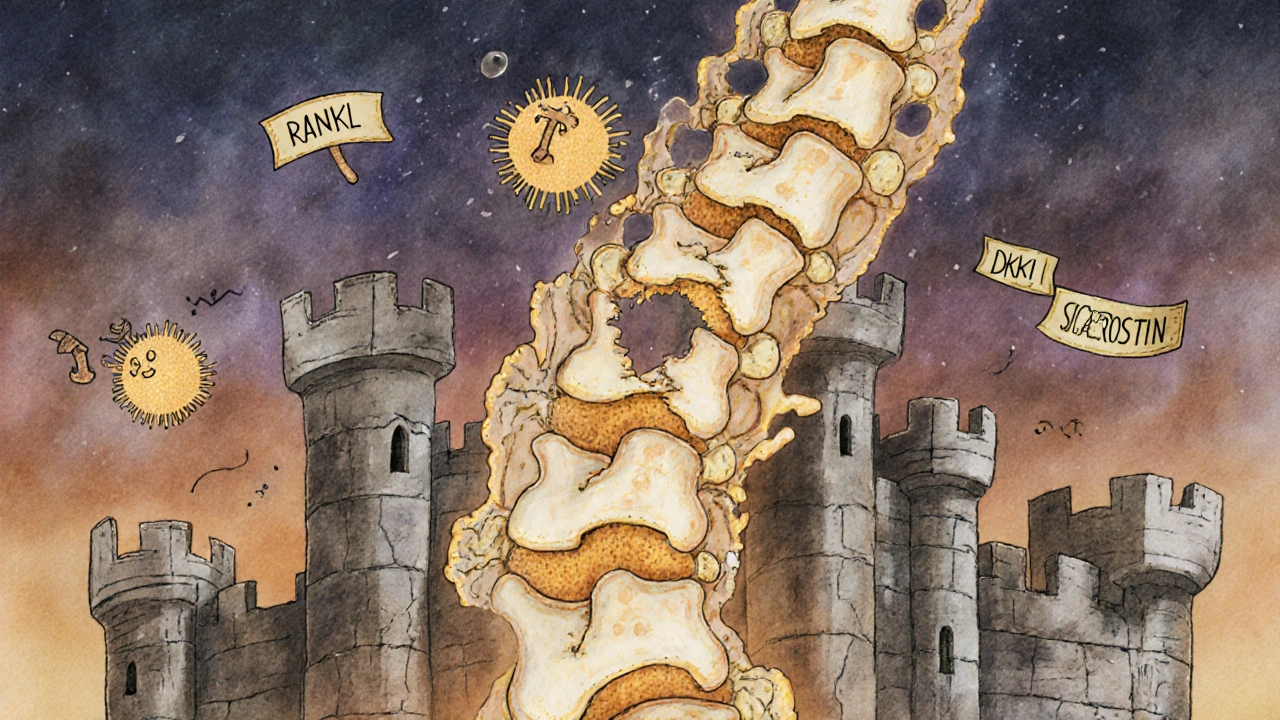
When your bones start to weaken, denosumab, a targeted biologic drug that stops bone breakdown by blocking a key protein called RANKL. Also known as Prolia, it's one of the most effective tools doctors use to protect bones in people with osteoporosis or cancer-related bone loss. Unlike older drugs that just add calcium or slow turnover, denosumab cuts the signal that tells bone-eating cells to destroy bone tissue. That means less breakage, fewer fractures, and more stability—especially for older adults or those on long-term steroids.
It’s not a daily pill. Denosumab comes as a simple injection, given once every six months by a nurse or doctor. That makes it easier to stick with than pills you have to remember every day. But it’s not for everyone. People with low calcium levels, kidney problems, or a history of jawbone issues need extra checks before starting. And if you stop it without switching to another bone drug, your bone loss can bounce back fast—sometimes even worse than before. That’s why it’s often paired with calcium and vitamin D, and why doctors watch your blood levels closely.
Denosumab doesn’t just help with osteoporosis. It’s also used in people with bone metastases from breast or prostate cancer, where tumors eat away at bone and cause pain or fractures. In those cases, it helps keep bones strong enough to handle daily life. It’s even used in rare conditions like giant cell tumor of bone, where abnormal cells destroy bone structure. The science behind it is precise: by blocking RANKL, it stops the chain reaction that leads to bone destruction at the cellular level.
What you won’t find in every doctor’s office is how denosumab stacks up against other treatments. Bisphosphonates like alendronate work differently—they stick to bone and kill off the cells that break it down. Denosumab doesn’t stick to bone; it works higher up, at the signal level. That’s why some patients switch when bisphosphonates stop working—or cause stomach issues. And while both help, denosumab often shows stronger bone density gains in clinical trials, especially in the spine and hip.
Side effects? Most people tolerate it well. But some get skin rashes, muscle pain, or infections. Rarely, it causes jawbone damage or unusual thigh fractures. That’s why you need regular check-ups, not just the injection. Your doctor will track your bone density, calcium levels, and overall health to make sure you’re getting the benefit without the risk.
Below, you’ll find real-world guides on how denosumab fits into broader treatment plans—from managing bone loss in cancer patients to understanding how it compares with other drugs like teriparatide or romosozumab. You’ll also see how it connects to things like calcium supplements, kidney health, and long-term monitoring. This isn’t just about the drug. It’s about how to use it safely, when to switch, and what to watch for after the injection.
Multiple Myeloma: Understanding Bone Disease and the New Treatments Changing Outcomes
- Beata Staszkow
- |
- |
- 8
Multiple myeloma causes severe bone damage in over 80% of patients. Learn how new drugs are moving beyond slowing bone loss to actually healing lesions, reducing fractures, and improving quality of life.
View more