Generic Drug Coverage: What You Pay, What You Get, and How to Save
When you hear generic drug coverage, the portion of your health plan that pays for medications that are chemically identical to brand-name drugs but cost far less. Also known as generic medication benefits, it’s one of the biggest ways your insurance helps you save money without sacrificing effectiveness. Most people don’t realize that generic drug coverage isn’t just a nice perk—it’s often the only reason they can afford their prescriptions at all. In 2024, generic drugs made up 90% of all prescriptions filled in the U.S. but accounted for just 12% of total spending. That’s not luck. That’s policy. And it’s why your copay for metformin might be $5 while the brand version costs $150.
But not all generic drug coverage, the portion of your health plan that pays for medications that are chemically identical to brand-name drugs but cost far less. Also known as generic medication benefits, it’s one of the biggest ways your insurance helps you save money without sacrificing effectiveness. is created equal. Some plans force you to try generics first before approving the brand. Others only cover certain generics—like the ones sold by the pharmacy chain they partner with. And if you’re on a high-deductible plan, you might pay full price until you hit your deductible, even if the drug is technically covered. That’s where prescription drug costs, the amount you pay out-of-pocket for medications, including copays, coinsurance, and deductibles, which vary widely based on insurance plan and drug type come into play. A $4 generic might still feel expensive if you’re paying $2,000 a year just to meet your deductible. Meanwhile, insurance coverage, the extent to which a health plan pays for medical services, including medications, procedures, and visits, based on plan terms and formulary rules can change from year to year. Your plan might drop coverage for a generic you’ve been using, or add a prior authorization step that delays your refill.
That’s why knowing your plan’s formulary matters. It’s not just a list of covered drugs—it’s a roadmap to your wallet. If your doctor prescribes a brand-name drug, ask if there’s a generic version on your plan’s list. If your pharmacy says your generic isn’t covered, call your insurer. Sometimes, it’s a billing error. Other times, you can file an exception. And if you’re paying cash, you might find the generic costs less than your copay. Stores like Walmart and Costco often sell common generics for under $5. You don’t need a coupon. You just need to ask.
Behind every cheap pill is a system designed to cut costs without cutting corners. Generic drugs must meet the same FDA standards as brand-name drugs. Same active ingredient. Same strength. Same way it works in your body. The only difference? No marketing budget. No patent. No fancy packaging. That’s why generic vs brand name drugs, the comparison between chemically identical medications where generics are lower-cost versions of brand-name drugs with identical efficacy and safety profiles isn’t a trade-off—it’s a win. You’re not settling. You’re smart.
Below, you’ll find real comparisons of medications people actually use—like Coumadin, Zoloft, Cialis, and amoxicillin—and how switching to generics saved them hundreds, sometimes thousands, a year. You’ll see how one person saved $200 a month just by switching from brand to generic warfarin. How another found a cheaper version of their antidepressant that didn’t cause weight gain. How people on blood thinners, diabetes meds, and ED drugs cut their costs without losing effectiveness. These aren’t theory pieces. These are real stories from real people who figured out how to make their coverage work for them.
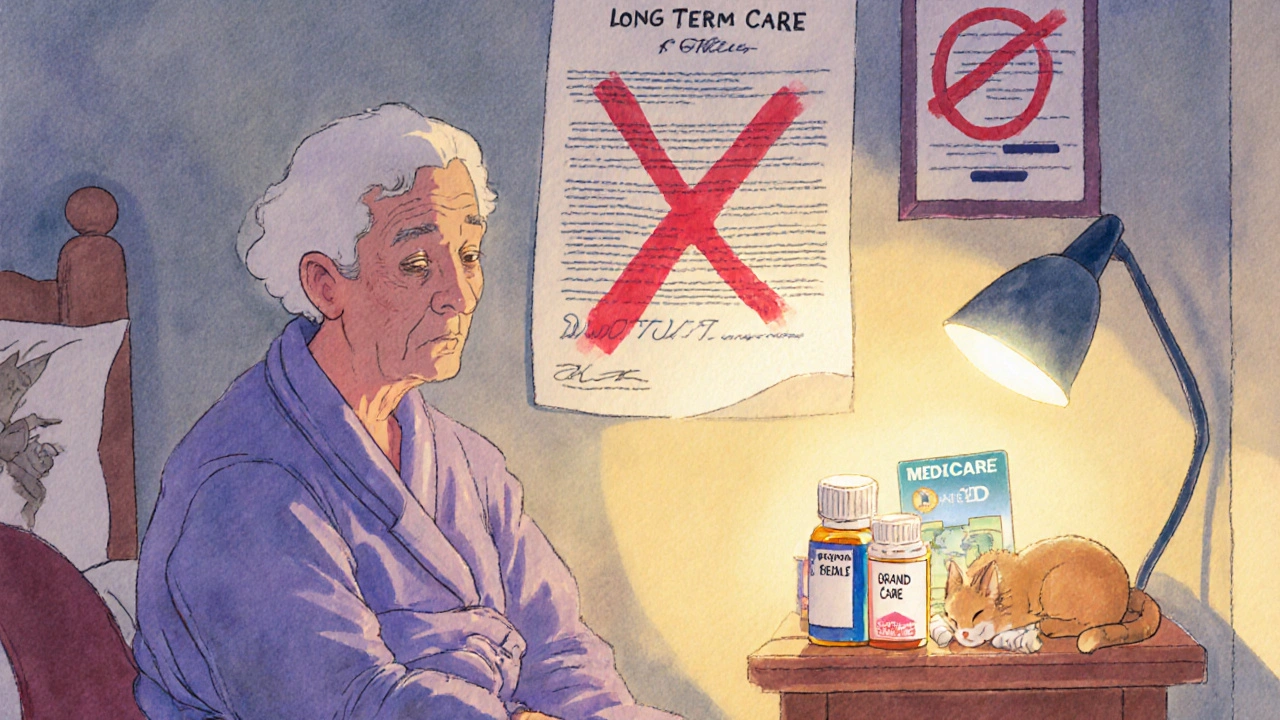
Long-Term Care Insurance and Generic Drug Coverage in Nursing Homes: What You Really Need to Know
- Beata Staszkow
- |
- |
- 9
Long-term care insurance doesn't cover generic drugs in nursing homes. Medicare Part D does - but formularies, delays, and enrollment gaps can block access. Know how it works to avoid costly surprises.
View moreHow Insurers Choose Which Generics to Cover
- Beata Staszkow
- |
- |
- 13
Insurers use P&T committees to choose generics based on clinical effectiveness, safety, and cost. Most are placed in Tier 1 with low copays. Learn how formularies work, why drugs get denied, and what to do if your medication isn't covered.
View more