Generic Drug Entry: What You Need to Know About Substitution, Savings, and Safety
When you pick up a prescription, the pill in your hand might not be the brand you asked for—that’s generic drug entry, the process by which FDA-approved versions of brand-name drugs enter the market at lower prices. Also known as generic substitution, it’s not just about saving money—it’s about making sure the right drug reaches the right person, at the right time, without compromising safety. Nearly 90% of prescriptions filled in the U.S. are for generics, but that doesn’t mean they’re all treated the same. Some states force pharmacists to swap brand names for generics unless you say no. Others let them do it only if your doctor doesn’t block it. And for drugs like insulin or seizure meds, where tiny differences matter, substitution is tightly controlled—or banned altogether.
The real power of generic drug entry, the process by which FDA-approved versions of brand-name drugs enter the market at lower prices. Also known as generic substitution, it’s not just about saving money—it’s about making sure the right drug reaches the right person, at the right time, without compromising safety. isn’t just in your wallet—it’s in the system. In 2024 alone, generics saved the U.S. healthcare system $482 billion. That’s money that didn’t go to pharmaceutical marketing, patent extensions, or executive bonuses. It went back into patient care, insurance premiums, and out-of-pocket costs. But here’s the catch: just because a generic is approved doesn’t mean your insurer will cover it. Insurance companies use P&T committees, Pharmacy and Therapeutics committees that decide which drugs go on formularies based on cost, safety, and clinical data. Also known as formulary review panels, they’re the unseen gatekeepers of your prescription coverage. They pick which generics make it to Tier 1 (lowest cost) and which get buried in higher tiers—or excluded entirely. And if your drug gets dropped from the formulary? You might pay 5x more, even if it’s the exact same chemical.
Then there’s the human side. Patients with chronic conditions—diabetes, high blood pressure, depression—rely on consistent dosing. Switching between generic manufacturers can sometimes trigger side effects, even when the active ingredient is identical. That’s why some doctors write "dispense as written" on prescriptions. And when it comes to NTI drugs, Narrow Therapeutic Index drugs where small changes in dosage can cause serious harm, like warfarin, levothyroxine, or phenytoin. Also known as narrow window medications, they require extra caution during substitution., the rules get stricter. Many states ban automatic substitution for these drugs. But not all. So if you’re on levothyroxine and move from Ohio to Texas, your pharmacy might swap your pill without telling you—and your thyroid levels could swing dangerously.
What you’ll find below isn’t just a list of articles. It’s a clear-eyed look at how generic drug entry really works—from the pharmacy counter to the statehouse, from your insurance formulary to the lab that tests whether a generic is truly interchangeable. You’ll learn how pharmacists decide what to swap, why some drugs are off-limits, how insurers choose which generics to cover, and what to do if your medication suddenly changes. Whether you’re managing a chronic condition, helping an aging parent navigate nursing home meds, or just trying to understand why your pill looks different this month, this collection gives you the facts—not the marketing.
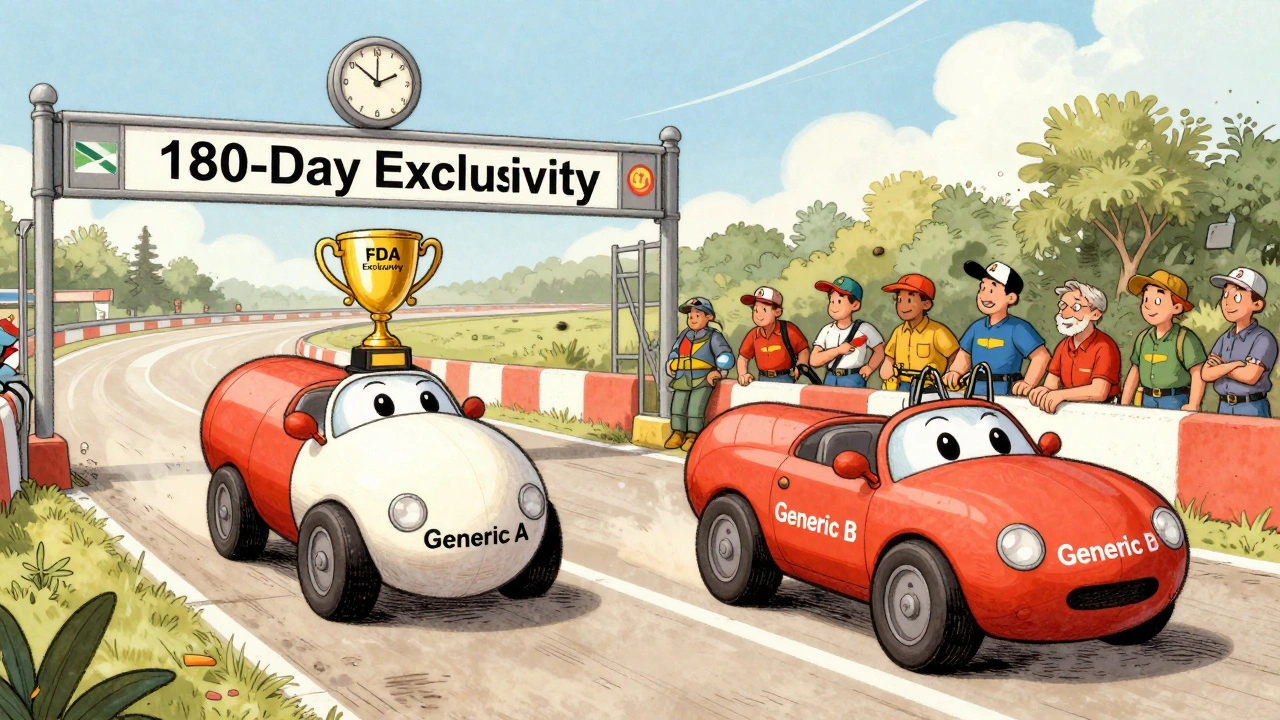
180-Day Exclusivity in Generic Drug Market Entry: How Patent Law Controls Access
- Keith Ashcroft
- |
- |
- 11
The 180-day exclusivity rule under the Hatch-Waxman Act gives the first generic drug maker to challenge a patent a temporary monopoly - but it often delays competition and keeps prices high. Here’s how it works, why it’s controversial, and what’s being done to fix it.
View more