Iron deficiency
When dealing with Iron deficiency, a condition where the body lacks sufficient iron to make healthy red blood cells. Also known as low iron, it can quietly sap energy and focus. Anemia, a reduced number of red blood cells often caused by iron deficiency is one of the most common outcomes. Doctors usually check Ferritin, the protein that stores iron in cells and reflects body iron stores to confirm the diagnosis, because low ferritin usually means the iron supply is running low. When the numbers dip, Iron supplements, tablet or liquid forms that help raise iron levels quickly become the first line of treatment. This trio—iron deficiency, anemia, and ferritin—forms the core framework you’ll encounter in every guide on the topic.
How diet, supplements, and testing connect
Understanding iron deficiency means looking at three intersecting pillars: what you eat, how you supplement, and how you measure. Iron‑rich foods like red meat, beans, and fortified cereals supply the heme and non‑heme iron that the gut absorbs. Heme iron from animal sources is absorbed at about 15‑35%, while non‑heme iron from plants tops out around 10%; vitamin C can boost that to nearly double. That’s why dietitians stress pairing beans with citrus or bell peppers. When diet alone isn’t enough—because of heavy menstrual loss, pregnancy, or gastrointestinal issues—medical professionals turn to iron supplements. Ferrous sulfate, gluconate, and fumarate are the most common forms; they differ in elemental iron content and side‑effect profiles. Taking a supplement with food reduces stomach upset but can also cut absorption, so timing matters. Testing ties the two together. A simple complete blood count (CBC) flags anemia, but the real iron story emerges from ferritin, transferrin saturation, and serum iron levels. Low ferritin confirms depleted stores, while normal ferritin with low hemoglobin might point to other causes. Some clinicians also order a reticulocyte hemoglobin content test to see how quickly the bone marrow is responding to therapy. Together, these labs guide whether you need a higher dose supplement, an IV infusion, or a dietary overhaul. For most adults, a daily iron supplement of 18 mg (the Recommended Dietary Allowance) keeps ferritin in the healthy range. People with diagnosed deficiency often need 60‑120 mg of elemental iron for several months, followed by a maintenance dose. Side effects like constipation or dark stools are common but manageable with fiber, hydration, or switching to a slower‑release formula. If oral therapy fails, doctors may prescribe intravenous iron, which bypasses the gut and restores ferritin rapidly. Beyond the basics, several lifestyle factors influence iron status. Chronic inflammation raises hepcidin, a hormone that blocks iron absorption, making ferritin appear falsely high. Regular vigorous exercise can increase iron loss through sweat and gastrointestinal bleeding, especially in endurance athletes. Even coffee or tea, rich in polyphenols, can shrink iron uptake if you sip them around meals. Recognizing these hidden culprits helps you fine‑tune both diet and supplement timing for optimal results. Putting it all together, the iron deficiency ecosystem revolves around three key entities: the condition itself, the diagnostic marker ferritin, and the corrective tool iron supplements. Each one interacts with diet, lifestyle, and lab testing, forming a loop that drives treatment decisions. Below you’ll find guides that break down each piece—how to spot early symptoms, which foods pack the most absorbable iron, how to choose the right supplement, and what lab results really mean. Whether you’re just curious about why you feel unusually tired, or you’ve been told you’re low on iron and need a clear plan, the articles ahead cover the full spectrum. From practical food swaps to step‑by‑step supplement protocols and interpreting test results, you’ll get the hands‑on info you need to tackle iron deficiency head‑on.
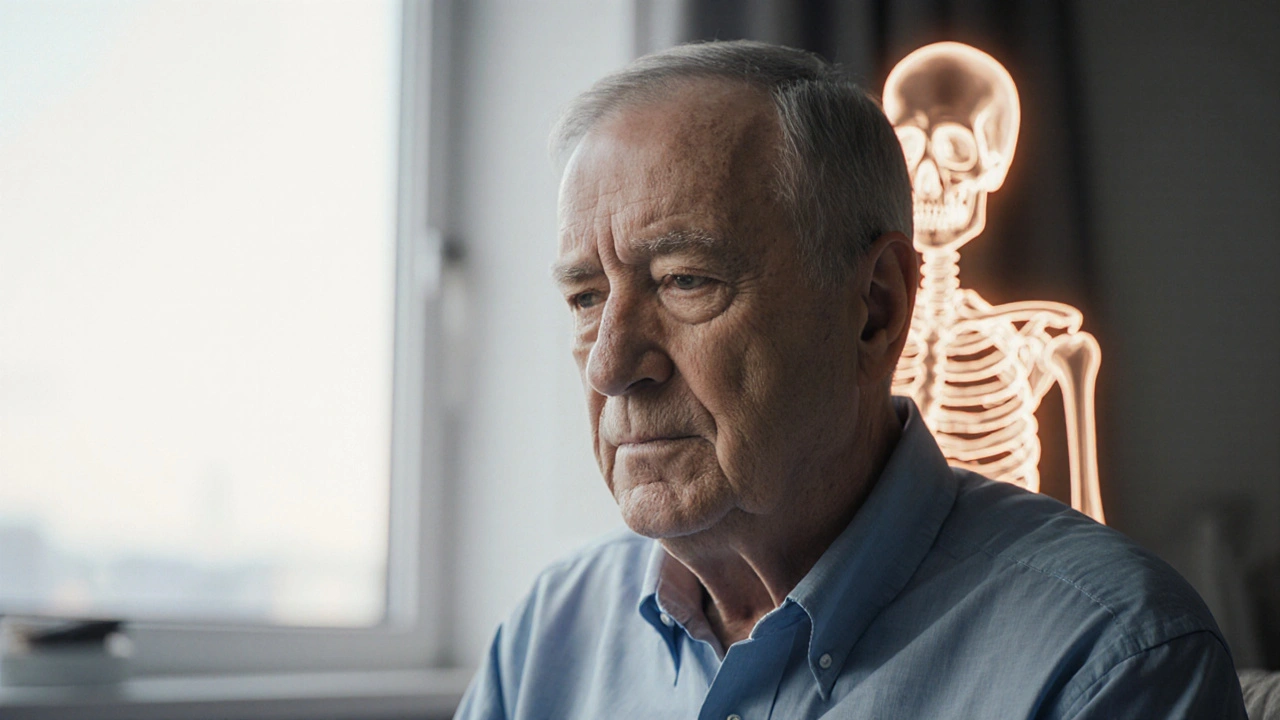
Anemia and Osteoporosis: How Low Blood Levels Affect Bone Health
- Keith Ashcroft
- |
- |
- 10
Explore how anemia influences bone health, the shared risk factors with osteoporosis, and practical steps to boost blood and bone strength.
View more