Novel Agents: What They Are and How They're Changing Treatment
When doctors talk about novel agents, newly developed drugs designed to target specific biological pathways that older medications can’t reach. Also known as targeted therapies, these medications are reshaping how we treat everything from cancer to autoimmune disorders and neurodegenerative diseases. Unlike older drugs that work broadly across the body, novel agents are built like precision tools—they lock onto a specific protein, gene, or cell type involved in disease. This means they often work better and cause fewer side effects.
These drugs aren’t just new versions of old ones. They’re built on breakthroughs in genetics, immunology, and molecular biology. For example, some novel agents block signals that tell cancer cells to grow, while others train the immune system to attack abnormal cells. In Parkinson’s, newer agents are being tested to slow nerve cell death instead of just masking symptoms. In psoriatic arthritis, they target the exact immune molecules that cause both skin and joint damage. Even in mental health, long-acting injectables are now being used as novel agents to improve adherence and stabilize outcomes for people with schizophrenia or bipolar disorder.
What makes these drugs different isn’t just how they work—it’s how they’re chosen. Doctors now look at genetic markers, disease subtypes, and even a patient’s history with other drugs before deciding if a novel agent is right. That’s why you’ll see posts here about things like fixed-dose combination drugs, mixing two or more medications in one pill to improve adherence and effectiveness. Also known as combination therapies, they’re often used with novel agents to boost results. Or why some posts warn about interactions—like how dopamine-blocking antiemetics can worsen Parkinson’s, because older drugs weren’t designed to work alongside these new targeted treatments.
But novel agents aren’t perfect. They’re expensive. They need careful monitoring. And sometimes, their long-term effects aren’t fully known yet. That’s why posts on this page cover everything from how insurers decide which ones to cover, to how they affect kidney function, or whether they’re safe during pregnancy. You’ll find comparisons between novel agents and older options, like how Avandia was replaced by safer diabetes drugs, or why Paxil is being swapped out for antidepressants with fewer side effects.
There’s also a growing focus on what happens after the drug is taken. Long-acting injectables mean side effects can linger for weeks, so monitoring isn’t optional—it’s essential. Environmental impacts matter too. Even antibiotics like tinidazole, once seen as harmless, are now being studied for how they pollute water and drive resistance. Novel agents aren’t just about treating disease—they’re forcing us to rethink how we use, pay for, and track every pill.
What you’ll find below isn’t a list of drug names. It’s a practical guide to understanding how these new treatments fit into real life—whether you’re managing heart failure, gout, COPD, or just trying to avoid dangerous interactions. These posts cut through the hype and show you what actually works, what to watch out for, and why some options are better than others—based on evidence, not marketing.
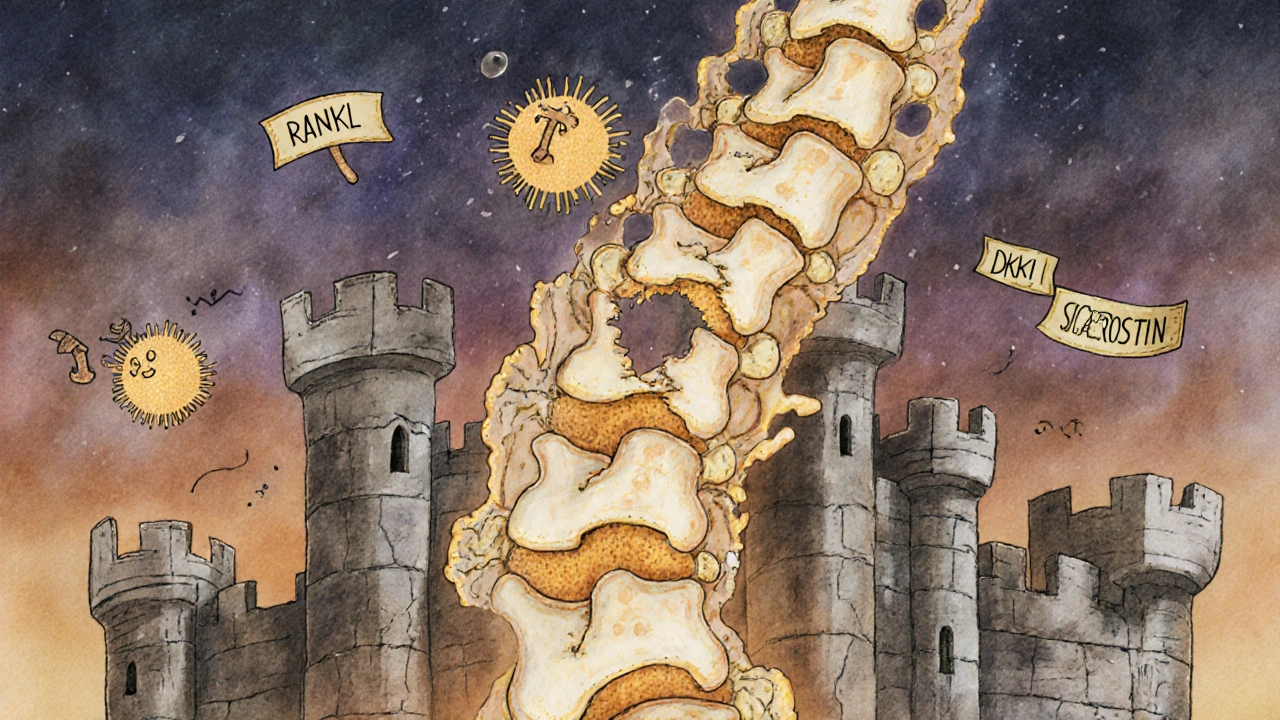
Multiple Myeloma: Understanding Bone Disease and the New Treatments Changing Outcomes
- Beata Staszkow
- |
- |
- 8
Multiple myeloma causes severe bone damage in over 80% of patients. Learn how new drugs are moving beyond slowing bone loss to actually healing lesions, reducing fractures, and improving quality of life.
View more