Medicare Part D: What It Covers, How It Works, and What You Need to Know
When you’re on Medicare Part D, the prescription drug coverage component of Medicare that helps pay for outpatient medications. Also known as Medicare drug plans, it’s not automatic—you have to enroll separately through private insurers approved by Medicare. Without it, you could be paying full price for everything from insulin to heart medications, even if you’re on a fixed income.
Medicare Part D works through drug formularies, lists of covered medications grouped into tiers with different costs. Each plan decides which drugs to include and how much you pay at the pharmacy. Some plans put generics on Tier 1 with $5 copays, while brand-name drugs might be Tier 3 or 4 with much higher costs. Not all drugs are covered—some plans exclude certain antidepressants, erectile dysfunction meds, or weight-loss pills. And if your drug isn’t on the list, you can ask for an exception, but it’s not guaranteed.
Costs aren’t just about the copay. There’s also a deductible, coverage gap (the infamous donut hole, a phase where you pay more out-of-pocket after spending a certain amount on drugs. In 2025, once you hit $5,000 in spending, you enter the donut hole), and catastrophic coverage that kicks in after you’ve spent a lot. Many people don’t realize they’re in the donut hole until they get a surprise bill. Low-income enrollees can get extra help paying for premiums and copays, but you have to apply—it doesn’t happen automatically.
Plans change every year. What was cheap last year might be off-formulary this year. Your insulin might switch from a $10 copay to $50. Your doctor might prescribe a new medication, and your plan won’t cover it. That’s why reviewing your plan during Open Enrollment (October 15 to December 7) isn’t optional—it’s critical. People who stick with the same plan year after year often end up paying hundreds more than they need to.
And it’s not just about the drug itself. Some plans require prior authorization before you can fill a prescription. Others limit how much you can get at once—like only 30 pills per month, even if your doctor writes for 90. If you take multiple meds, you might need to switch to a different brand just to fit your plan’s rules. That’s why knowing your plan’s rules matters as much as knowing your meds.
You’ll find posts here that explain how insurers pick which generics to cover, how state laws affect whether pharmacists can swap brands for cheaper versions, and how to balance medication use with side effects like low potassium or dehydration. These aren’t random articles—they’re all connected to the real-world challenges of getting your prescriptions covered, affordable, and safe under Medicare Part D. Whether you’re helping a parent navigate their first year on Medicare, managing your own chronic condition, or just trying to avoid surprise bills, the information below will help you make smarter choices—without the jargon.
Medicare Part D Drug Coverage Explained for Patients in 2025
- Beata Staszkow
- |
- |
- 12
Medicare Part D in 2025 now caps out-of-pocket drug costs at $2,000 annually, eliminating the donut hole. Learn how the new coverage phases work, how to choose a plan, and what you still need to watch for.
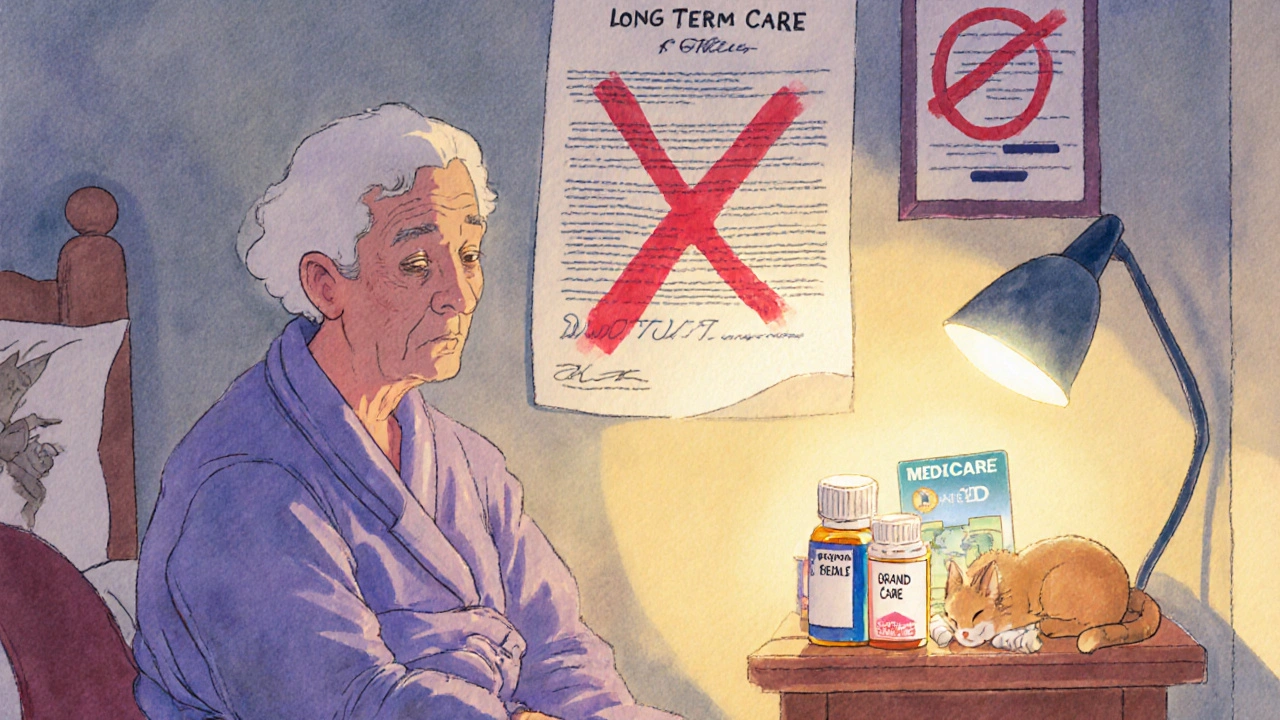
View moreLong-Term Care Insurance and Generic Drug Coverage in Nursing Homes: What You Really Need to Know
- Beata Staszkow
- |
- |
- 9
Long-term care insurance doesn't cover generic drugs in nursing homes. Medicare Part D does - but formularies, delays, and enrollment gaps can block access. Know how it works to avoid costly surprises.
View more