Prescription Drug Coverage: What’s Covered, Why It Matters, and How to Fight Denials
When you walk into a pharmacy with a prescription, what you pay isn’t just about the drug—it’s about prescription drug coverage, the set of rules your health plan uses to decide which medications it will pay for and at what cost. Also known as formulary coverage, it’s the invisible gatekeeper between your doctor’s order and your medicine bottle. Most people assume if a drug is FDA-approved, it’s covered. That’s not true. Insurers use P&T committees, pharmacy and therapeutics panels made up of doctors and pharmacists who review drugs for safety, cost, and clinical value to build their lists. These committees don’t care if a drug is brand new or heavily advertised. They care if it’s better than cheaper alternatives—and often, it’s not.
Generic drugs, medications that are chemically identical to brand-name versions but cost far less dominate these lists. Why? Because they save billions. In 2024, generics made up 90% of prescriptions but only 12% of spending. That’s why most formularies put them in Tier 1—with the lowest copay. But coverage doesn’t stop there. Tiered formularies, a system that ranks drugs by cost and clinical value, placing them in tiers from lowest to highest out-of-pocket expense mean your drug’s price depends on where it lands. A brand-name drug might be in Tier 3 or 4, meaning you pay 30-50% of the cost. Even if your doctor insists on it, your insurer might require you to try a generic first. That’s step therapy—and it’s legal, common, and often frustrating.
When your drug gets denied, it’s not always about cost. Sometimes it’s about policy. Insurers may block a drug because it’s used off-label, because there’s a cheaper alternative they prefer, or because they’ve never reviewed it properly. But you have rights. You can appeal. You can ask your doctor to write a letter of medical necessity. You can check if your plan has an exception process. And you can always ask your pharmacist to check if a similar drug on formulary might work just as well. This collection of articles dives into exactly how these systems work—from how insurers choose which generics to cover, to how state laws force or allow substitutions, to why some drugs get left off the list entirely. You’ll find real examples of denials, fixes, and workarounds. No fluff. No jargon. Just what you need to know to get the meds you’re prescribed—and not pay more than you have to.
Medicare Part D Drug Coverage Explained for Patients in 2025
- Beata Staszkow
- |
- |
- 12
Medicare Part D in 2025 now caps out-of-pocket drug costs at $2,000 annually, eliminating the donut hole. Learn how the new coverage phases work, how to choose a plan, and what you still need to watch for.
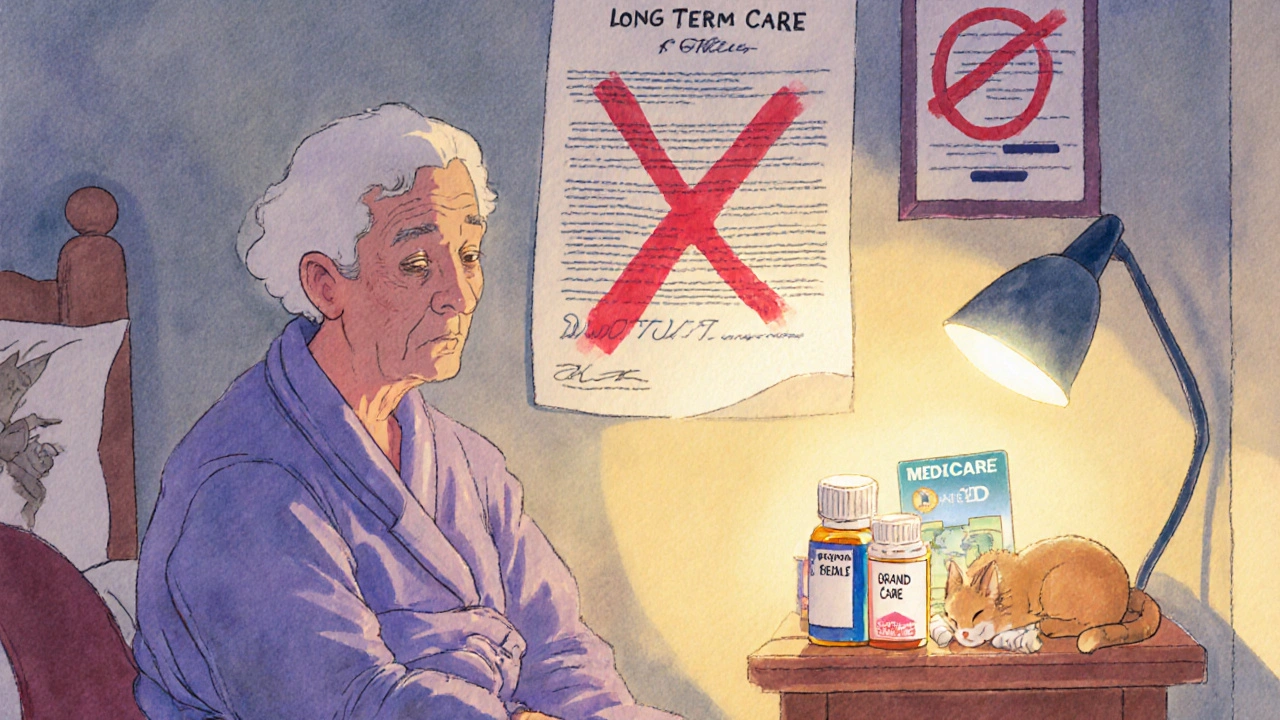
View moreLong-Term Care Insurance and Generic Drug Coverage in Nursing Homes: What You Really Need to Know
- Beata Staszkow
- |
- |
- 9
Long-term care insurance doesn't cover generic drugs in nursing homes. Medicare Part D does - but formularies, delays, and enrollment gaps can block access. Know how it works to avoid costly surprises.
View more