Generic Substitution: Save Money Without Sacrificing Effectiveness
When you hear generic substitution, the practice of replacing a brand-name drug with a chemically identical generic version. Also known as generic switching, it’s one of the simplest ways to cut your pharmacy bill without losing effectiveness. Most people think brand-name drugs are better—maybe because they cost more, or because they’ve seen the ads. But the truth? The FDA requires generics to have the same active ingredient, strength, dosage form, and performance as the original. That means generic substitution isn’t a compromise—it’s a smart upgrade.
It’s not just about saving a few dollars. In 2024, generic drugs saved the U.S. healthcare system over $482 billion by making up 90% of prescriptions but only 12% of total spending. That’s billions going back into patients’ pockets, insurance funds, and public health programs. And it’s not just pills—biosimilars, complex biologic drugs that mimic expensive biologics like Humira or Enbrel are now entering the market, with potential to cut another $234 billion in the next few years. But for most people, the real savings come from everyday brand name drugs, medications sold under a company’s trademark, like Paxil, Coumadin, or Cialis. Also known as name-brand medications—the ones you’ve been paying full price for, even though a generic version has been available for years.
Generic substitution works because the law requires it. Pharmacists can swap a brand drug for its generic unless your doctor writes "dispense as written" or your state blocks automatic substitution. But many people don’t know this. They see the brand name on the bottle and assume it’s the only option. That’s why so many still pay $200 for a brand-name pill when the generic costs $10. The same active ingredient. Same side effects. Same results. The only difference? The label. And sometimes, the color of the pill.
Look at the posts below. You’ll see real comparisons: Avandia vs metformin, Paxil vs Zoloft, Coumadin vs warfarin, Cialis vs Tadora. These aren’t random lists—they’re proof that generic substitution isn’t theoretical. It’s happening every day, in clinics and pharmacies across the country. People are switching to generics for gout, depression, diabetes, ED, and even eye drops. And they’re not losing anything. In fact, many feel better because they can finally afford to take their meds consistently.
Some doctors still hesitate to recommend generics—old habits, unclear guidelines, or pressure from reps. But you don’t need their permission. You just need to ask. "Is there a generic version?" is one of the most powerful questions you can ask at the pharmacy counter. It doesn’t make you cheap. It makes you informed. And with the right knowledge, you can take control of your health without taking on debt.
Combination NTI Drugs and Generic Availability: Coverage and Gaps
- Keith Ashcroft
- |
- |
- 12
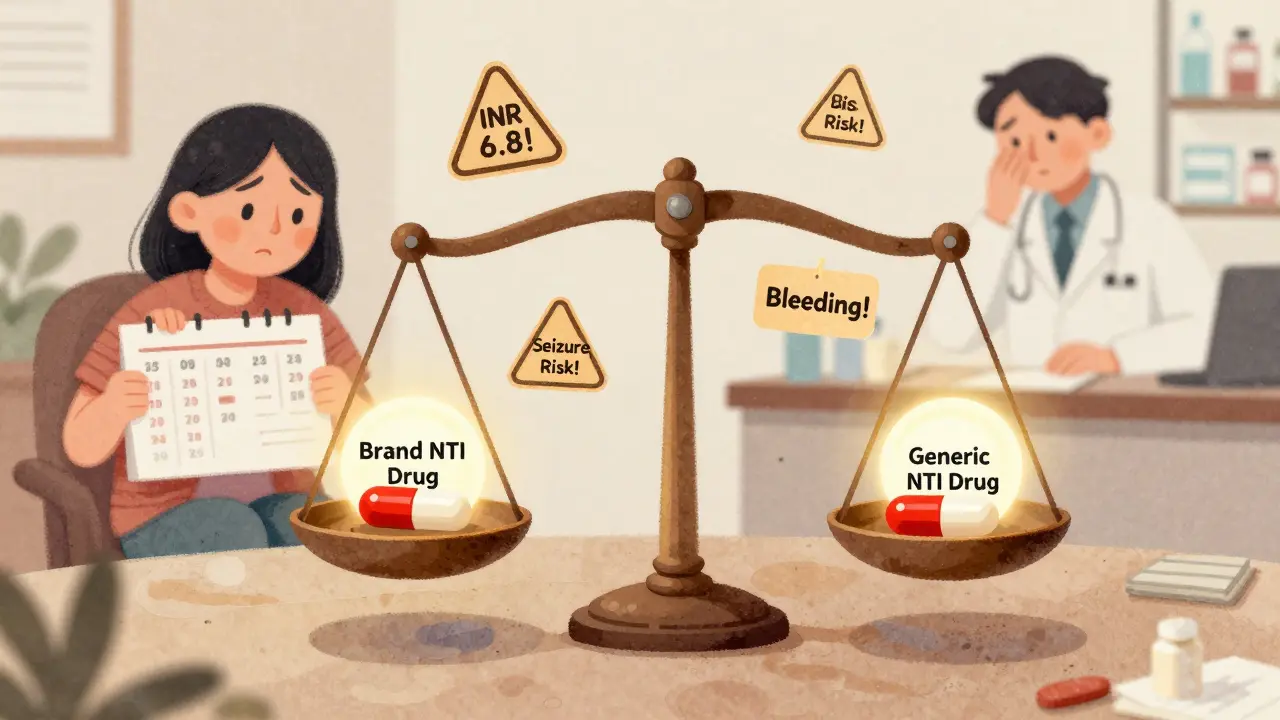
Combination NTI drugs offer powerful treatment for complex conditions, but generic versions are nearly nonexistent due to strict bioequivalence requirements and high safety risks. Patients face gaps in access and monitoring, with real-world consequences.
View moreState Laws on Generic Drug Substitution: What Pharmacists and Patients Need to Know
- Keith Ashcroft
- |
- |
- 10
State laws on generic drug substitution vary widely across the U.S., affecting how pharmacists swap brand-name drugs for generics. Learn how consent rules, NTI drug restrictions, and biosimilar policies differ by state-and what patients and pharmacists need to know.
View moreHow Insurers Choose Which Generics to Cover
- Beata Staszkow
- |
- |
- 13
Insurers use P&T committees to choose generics based on clinical effectiveness, safety, and cost. Most are placed in Tier 1 with low copays. Learn how formularies work, why drugs get denied, and what to do if your medication isn't covered.
View more